Losing your hair is rarely just about the hair itself. More often than not, it's a sign that something is going on with your scalp. From inflammatory conditions like psoriasis to hormonal shifts, a whole host of scalp conditions that cause hair loss can knock your hair's natural growth cycle off kilter. Figuring out that root cause is always the first, most important step toward getting things back on track.
Why a Healthy Scalp Is Your Hair's Foundation
We spend a lot of time focused on the hair we can see, but the real magic happens at the root. Think of your scalp as the soil in a garden—if the soil is unhealthy and depleted of nutrients, you’ll never grow strong, vibrant plants. It's the exact same concept for your hair. Every single strand sprouts from a follicle, a tiny pocket in the skin that needs a healthy, balanced environment to do its job.
This is precisely where trouble usually starts. When your scalp is stressed by inflammation, an infection, or even hormonal fluctuations, it undermines the very foundation your hair relies on. The fallout? Hair thinning, excessive shedding, or even bald patches.
The Hair Growth Cycle Explained
To really grasp how things go wrong, you first need to understand how hair is supposed to grow. Every follicle on your head follows a predictable, repeating cycle with three key phases:
- Anagen (Growth Phase): This is the main event, when your hair is actively getting longer. This phase can last anywhere from 2 to 7 years, and it’s what determines your hair’s maximum length.
- Catagen (Transition Phase): A very brief pit stop, this phase only lasts a couple of weeks. The hair follicle shrinks and detaches from the blood supply, preparing to rest.
- Telogen (Resting Phase): For about three months, the follicle is dormant. At the end of this phase, the old hair strand is shed to make way for a new one, and the anagen phase starts all over again.
In a healthy scalp, about 85-90% of your hair is in the anagen phase at any one time. This balance is what keeps your hair looking full and thick.
How Scalp Issues Disrupt the Cycle
The different scalp conditions that lead to hair loss essentially sabotage this finely tuned cycle. For instance, widespread inflammation can shock follicles, forcing them to jump from the growth phase straight into the resting phase. This leads to a sudden, noticeable increase in shedding, a condition known as telogen effluvium.
A compromised scalp creates an environment where hair follicles can't function properly. Whether it's due to inflammation, infection, or hormonal interference, the result is a disruption of the natural growth cycle, leading to visible hair loss.
In more severe cases, like with scarring alopecias, the follicle itself can be permanently damaged or destroyed. When that happens, no new hair can grow from that spot. By treating hair loss as a symptom, you can shift your focus to finding and fixing the real problem on your scalp. In this guide, we'll walk through the most common culprits.
The Common Culprit: Androgenetic Alopecia

When you look in the mirror and notice a widening part or a hairline that’s starting to retreat, you’re likely seeing the work of Androgenetic Alopecia (AGA). It’s the single most common reason people lose their hair, though you probably know it better as male or female pattern baldness. This isn't an illness in the typical sense; it's a slow, predictable process dictated by your genes and hormones.
The story of AGA unfolds over years, not overnight. It’s a quiet, gradual thinning that often flies under the radar until it becomes pretty obvious. That’s what makes it so frustrating—it’s easy to miss the early signs, only to feel like the change happened all at once when you finally see it.
The Science Behind Pattern Hair Loss
At the root of Androgenetic Alopecia is a potent hormone called dihydrotestosterone (DHT), which is derived from testosterone. If you have the genetic predisposition, the hair follicles on your scalp are extra sensitive to this hormone. Think of DHT as a key that perfectly fits the locks on these sensitive follicles; once it connects, it sends a signal for the follicle to shrink.
This shrinking process is called miniaturization. Over time, DHT’s constant signaling causes the affected follicles to get smaller and smaller. With each new growth cycle, the hair that emerges is shorter, finer, and weaker. Eventually, the follicle may shrink so much that it stops producing a visible hair altogether.
The real problem in Androgenetic Alopecia isn't that hair is falling out—it's that the follicles themselves are shrinking. This miniaturization process slowly replaces thick, healthy hair with fine, almost invisible "peach fuzz," which creates the appearance of thinning and baldness.
The sheer number of people dealing with AGA is astounding. It’s the leading cause of hair loss worldwide, impacting roughly 85% of men and 33% of women during their lifetime. To put that in perspective, in the United States alone, an estimated 50 million men and 30 million women are living with this genetic reality.
How AGA Looks Different in Men and Women
Even though DHT and genetics are the universal drivers, AGA shows up differently depending on your sex. The patterns are so distinct, in fact, that experts use specific scales to classify them—the Norwood scale for men and the Ludwig scale for women.
For men, the progression is often very predictable:
- A Receding Hairline: It almost always begins with thinning at the temples, which carves out that classic "M" shape.
- Thinning at the Crown: Around the same time, a bald spot often starts to form on the back of the head, or the vertex.
- Merging and Expansion: Over the years, these two areas of loss tend to expand until they meet, leaving just a horseshoe-shaped ring of hair around the sides and back.
For women, the experience is usually more widespread and subtle:
- Diffuse Thinning: Instead of a receding hairline, women typically experience a gradual, diffuse thinning all over the top of the scalp.
- A Widening Part: Often, the very first sign is a widening of the center part, which makes more of the scalp visible through the hair.
- The Hairline Stays Put: Unlike men, women with AGA generally keep their frontal hairline intact.
Recognizing these patterns is the first step toward taking action. If any of this sounds familiar, you can start to dig deeper. For a more detailed breakdown, you can learn more by reading our complete guide on what is androgenetic alopecia. Having this knowledge moves you from simply worrying about thinning hair to understanding—and addressing—the root cause.
How Inflammation Triggers Hair Thinning
That constant itch or persistent flaking on your scalp is more than just an annoyance. It’s often your body's alarm bell for inflammation, a process that can directly throw a wrench in your hair's growth cycle. When your scalp is in a state of constant irritation, it becomes a hostile environment for hair follicles, which can lead to significant shedding and thinning over time.
Two of the most common culprits behind inflammation-driven hair loss are Seborrheic Dermatitis and Scalp Psoriasis. While both leave your scalp feeling irritated, they're actually very different problems with unique triggers. Figuring out which one you're dealing with is the critical first step toward getting the right help.
Seborrheic Dermatitis: The Overactive Yeast Connection
Think of seborrheic dermatitis as a severe, angry form of dandruff. It’s triggered by an overgrowth of a yeast called Malassezia, a microorganism that lives on most adult skin without causing any trouble. In some people, however, the immune system overreacts to its presence, launching an inflammatory attack that results in those all-too-familiar symptoms.
This condition loves to show up where oil glands are most active—like your scalp, face, and chest. On the scalp, it typically looks like:
- Greasy, yellowish flakes that seem to cling to the hair and scalp.
- Red, inflamed skin hiding underneath the flaky patches.
- Persistent itching that can become incredibly intense during a flare-up.
The constant scratching and the underlying inflammation team up to disrupt the hair follicles, pushing them into the shedding phase way too early. When this cycle of irritation becomes chronic, it can weaken the follicles and lead to noticeable hair thinning. For a more detailed look, you might find our guide on what seborrheic dermatitis is and how it affects hair helpful.
Scalp Psoriasis: An Autoimmune Mix-Up
Scalp psoriasis, on the other hand, is an autoimmune issue. Put simply, the body’s own immune system gets its signals crossed and mistakenly attacks healthy skin cells. This assault forces them to multiply at a super-speed—we're talking days instead of weeks. The result is a buildup of thick, scaly patches known as plaques.
Unlike the oily, yellowish flakes from seborrheic dermatitis, psoriasis plaques are quite distinct:
- Thick, silvery-white scales sitting on top of well-defined red patches of skin.
- Dry texture that's often prone to cracking or even bleeding.
- A tendency to extend beyond the hairline onto the forehead, neck, or behind the ears.
The inflammation here runs deep, damaging hair follicles and making it tough for hair to thrive. The thick scales can also physically block new hairs from emerging. Worse, trying to pick off or remove the plaques can easily pull out healthy hairs along with them, creating temporary bald spots.
This image shows just how an autoimmune response can lead directly to follicle damage and patchy hair loss.
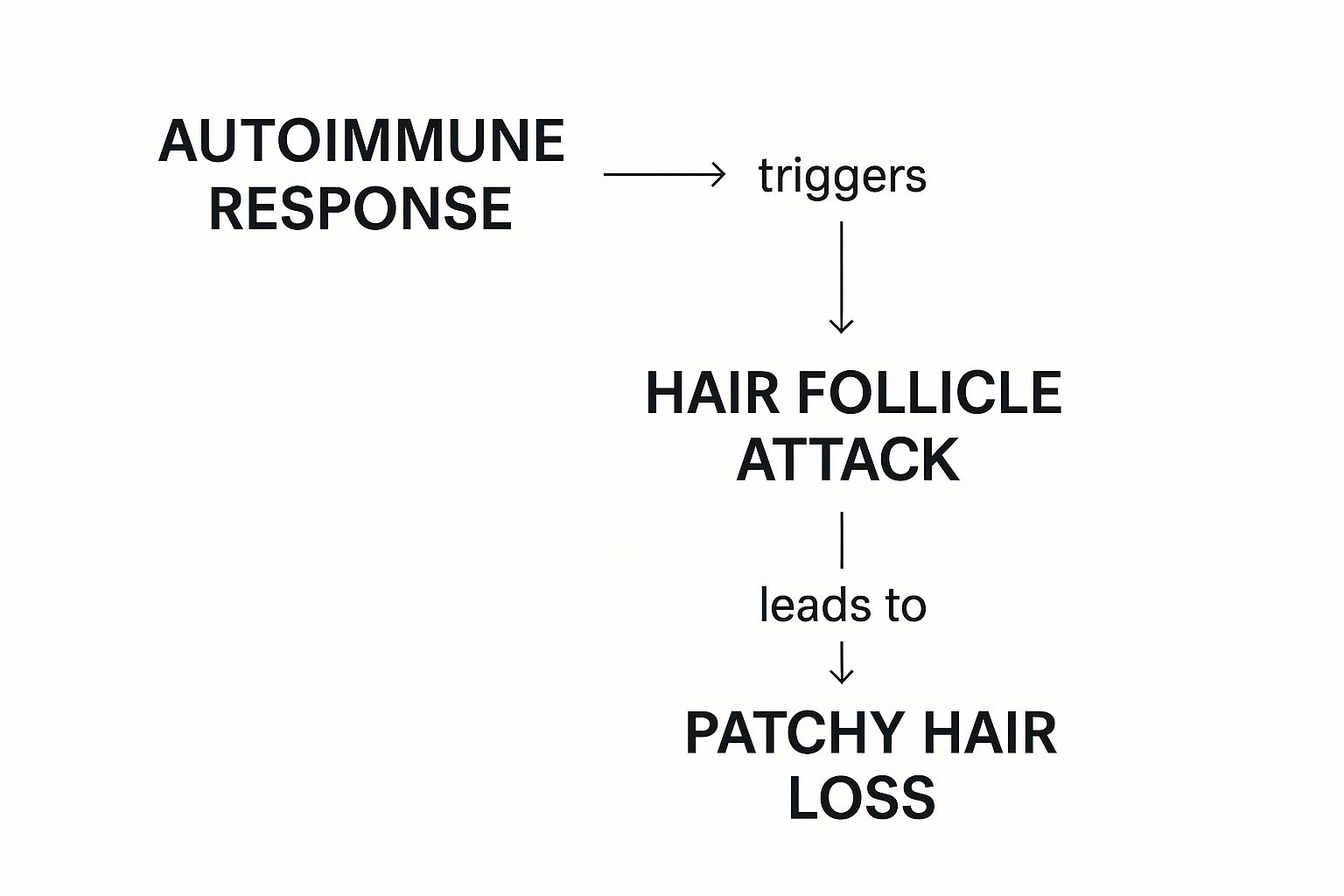
As you can see, when the immune system mistakenly targets the follicles, the direct consequence is hair falling out in specific areas.
To help you tell these conditions apart, here's a quick comparison.
Comparing Inflammatory Scalp Conditions
| Feature | Seborrheic Dermatitis | Scalp Psoriasis | Common Dandruff |
|---|---|---|---|
| Flake Appearance | Greasy, yellowish, and often sticky | Thick, silvery-white, and dry | Small, white or yellowish, and oily or dry |
| Skin Appearance | Red, inflamed, and oily | Red, thick, and well-defined patches (plaques) | Can be slightly red or look normal |
| Common Location | Scalp, face (eyebrows, nose), chest, back | Scalp, elbows, knees, lower back | Primarily on the scalp |
| Main Sensation | Persistent itching | Itching, burning, or soreness | Mild to moderate itching |
| Underlying Cause | Overreaction to Malassezia yeast | Autoimmune response | Mild reaction to Malassezia or dry skin |
This table clarifies that while they might all seem like "bad dandruff" at first glance, the underlying causes and symptoms are very different, which is why a proper diagnosis is so important.
The Real Impact of Itch and Flakes
It’s easy to write off flaking and itching as minor problems, but they are often signs of a bigger issue. Conditions like dandruff and seborrheic dermatitis create chronic irritation that can lead to hair loss. In fact, dandruff affects a huge portion of the population—between 5% and 10% globally.
In places like Europe and the US, it's a top concern, with about 17% of people reporting it. All that relentless itching leads to scratching, which physically damages both the scalp's protective barrier and the hair strands themselves, causing breakage and shedding.
The core issue isn't just the visible flakes. The real enemy is the hidden inflammation that messes with the hair growth cycle and weakens follicles from the inside out. If left unchecked, hair loss is an almost inevitable result.
Getting that inflammation under control is priority number one. When you calm the scalp, you're restoring a healthy environment where your hair follicles can finally get back to work. This not only stops the excessive shedding but also gives your hair a real chance to regrow stronger than before.
When Your Body Becomes the Problem

While many scalp problems are caused by things like fungus or inflammation, sometimes the real issue is coming from inside your own body. These conditions can be incredibly frustrating because your body's own systems—the very ones meant to protect you—start working against your hair follicles.
This is where things get complicated. Without a professional eye, it’s tough to figure out what’s really going on. Let's look at two prime examples of this: Alopecia Areata and Folliculitis. One is a case of mistaken identity, and the other is an infection that spirals out of control.
Alopecia Areata: The Friendly Fire Problem
Alopecia Areata is a classic autoimmune condition. Think of your immune system as a highly trained security team protecting your body from viruses and bacteria. In a person with Alopecia Areata, this security team gets bad intel and misidentifies your healthy hair follicles as dangerous intruders.
What happens next is essentially a "friendly fire" incident. Immune cells swarm the hair follicles, causing inflammation that slams the brakes on hair production. The good news is this attack usually doesn't destroy the follicle itself; it just forces it into a dormant state. This leads to hair falling out in very distinct, smooth, round patches that can pop up suddenly on your scalp, beard, or anywhere else on your body.
With Alopecia Areata, the immune system isn't demolishing the hair factory (the follicle); it's just cutting the power. That's why, with the right approach to calm the immune response, hair can often regrow completely.
Scientists are still working to understand the exact triggers, but it’s believed to be a mix of genetics and environmental factors. It’s a perfect example of an internal system going haywire. It's also important to note this isn't the same as hormonally-driven hair loss. To see how different internal signals can cause hair thinning, check out our guide on hair loss hormonal imbalance.
Folliculitis: When Follicles Get Infected
Folliculitis is a different beast altogether—it’s an infection. Every single hair on your head grows from a tiny pocket in the skin called a follicle. When these follicles get blocked or damaged from things like friction or shaving, they become a prime target for bacteria (usually Staphylococcus aureus), yeast, or fungi.
Once these invaders get in, your body launches an inflammatory counter-attack. The result? Small, itchy, and often painful bumps that look a lot like an acne breakout on your scalp.
Folliculitis isn't a one-size-fits-all condition. It can show up in a few different ways:
- Superficial Folliculitis: This type only affects the upper part of the follicle. You’ll see small red bumps or whiteheads that typically heal without leaving a scar.
- Deep Folliculitis: This is much more serious because the infection goes all the way down the follicle. It can create large, painful boils or cysts that burrow deep into the skin.
If a deep infection is ignored, the inflammation can become so severe that it permanently destroys the hair follicle. This is how scarring alopecia develops, leaving behind bald patches where hair will never grow back. This is why getting on top of folliculitis early is absolutely critical—you're in a race to save the follicle before the damage is done for good.
Ultimately, whether it's an autoimmune mix-up or a bacterial invasion, getting the right diagnosis is the only way forward. A dermatologist can pinpoint the true cause, helping you find a path to restoring your scalp's health and stopping hair loss in its tracks.
Getting an Accurate Hair Loss Diagnosis
Trying to pinpoint the exact scalp condition causing your hair loss can feel like you're just guessing in the dark. Going down the rabbit hole of online self-diagnosis usually just leads to more stress and confusion. That’s why getting a professional opinion from a dermatologist or a trichologist—a specialist who lives and breathes hair and scalp health—is absolutely essential. It’s the only way to swap that guesswork for a real, evidence-based plan.
The first thing any good specialist will do is simply talk to you. This initial conversation is a huge piece of the puzzle. They'll ask about your medical history, whether hair loss runs in your family, your diet, recent stress, and any medications you’re on. Think of it as detective work; these details are the first clues that help narrow down the long list of possibilities.
The Physical Scalp Examination
After getting your story, the specialist will get hands-on with a thorough examination of your hair and scalp. They aren't just looking for thinning areas. They're meticulously analyzing the pattern of the hair loss, and checking for tell-tale signs like inflammation, scaling, redness, or even scarring.
To get a closer look, they'll almost certainly use a dermatoscope. This is basically a high-powered magnifying glass made specifically for skin. It lets them see your hair follicles and the surrounding scalp in incredible detail, helping them spot things the naked eye would miss—like the miniaturized hairs seen in androgenetic alopecia or the unique "exclamation point" hairs that are a hallmark of alopecia areata.
A professional diagnosis is all about connecting the dots between your personal history and the physical evidence on your scalp. It’s a systematic investigation, ruling out one possibility at a time until the real culprit is found.
Sometimes, just looking isn't enough to solve the mystery. If your symptoms suggest there might be an underlying medical issue, an autoimmune condition, or a nutrient deficiency at play, your doctor will likely order a few more tests for definitive answers.
Advanced Diagnostic Tools
When the cause still isn't crystal clear, specialists have a few more tricks up their sleeve to dig deeper. These tests give them the hard data needed to confirm what they suspect.
- Blood Tests: A simple blood draw can tell a surprisingly detailed story. Your doctor might check your thyroid function, iron and ferritin levels, vitamin D, or specific hormones to make sure an internal imbalance isn't triggering your hair loss.
- Scalp Biopsy: For more complex situations, especially if a scarring alopecia is a possibility, a scalp biopsy might be the next step. It sounds scarier than it is—it just involves taking a tiny skin sample (about 4mm) from your scalp for lab analysis. The area is numbed, and it’s a very quick procedure.
This microscopic look at the tissue gives a conclusive answer, showing exactly what’s happening to the hair follicles below the surface. To get a better sense of what this involves, you can learn more about the role of a scalp biopsy for hair loss in our dedicated guide.
Ultimately, getting a real diagnosis is empowering. It breaks the cycle of worry and trying random products that don't work. It puts you on the right path toward a treatment that actually has a chance of success. For anyone looking for a clear path forward, this guide offers comprehensive hair loss treatment tips. Remember, getting the right diagnosis isn't just a step—it's the most critical first step you can take.
Modern Treatments for Scalp and Hair Health
Finally getting a diagnosis is a huge relief. It moves you from a place of uncertainty to one where you can actually start taking action. When it comes to treating the various scalp conditions that cause hair loss, the options are incredibly varied, ranging from simple medicated shampoos to sophisticated clinical procedures. The best path forward always hinges on the specific cause, but the end goal is universal: get your scalp back in balance so your hair has a healthy environment to thrive.
For many people, the journey starts with specialized shampoos. Don't think of these as just cleansers; they're more like targeted scalp therapies, packed with active ingredients designed to tackle the problem at its source.
Over-the-Counter and Prescription Solutions
If inflammation is the main culprit—as it is with seborrheic dermatitis or scalp psoriasis—the right medicated shampoo can be a game-changer. Key ingredients like ketoconazole, selenium sulfide, and coal tar work hard to get yeast under control, slow down the rapid turnover of skin cells, and soothe irritation.
- Ketoconazole: This is a powerful antifungal that goes after the Malassezia yeast, the microbe behind seborrheic dermatitis and stubborn dandruff. By reining in the fungal population, it effectively reduces the frustrating flaking and itching. To learn more, our guide on how ketoconazole shampoo combats hair loss breaks it all down.
- Topical Minoxidil: When you're dealing with androgenetic alopecia (genetic hair loss), minoxidil is usually the first thing a doctor will suggest. It's a vasodilator, which is a fancy way of saying it widens the blood vessels in your scalp. This boosts blood flow to the follicles and helps extend their anagen, or active growth, phase.
Just remember, consistency is everything with these treatments. For instance, studies on minoxidil show that it can take up to one year of continuous daily use to see its peak effects.
The most effective treatments are those that directly address the specific cause of your hair loss. An antifungal won't help genetic thinning, and a growth stimulant won't fix an autoimmune attack. This is why an accurate diagnosis is non-negotiable.
Advanced and Regenerative Therapies
Sometimes, topicals just don't cut it, or the condition calls for a more powerful approach. That's when doctors might bring in more advanced options, like prescription medications or innovative procedures that work on a deeper level.
For autoimmune conditions like Alopecia Areata, corticosteroids are a go-to. These potent anti-inflammatories can be applied as a cream, injected directly into the bald patches on the scalp, or even taken as a pill to calm the immune system’s misguided attack on the hair follicles.
More recently, the field of regenerative medicine has opened up an exciting new front: Platelet-Rich Plasma (PRP) therapy. The process is straightforward: a small amount of your own blood is drawn, spun in a centrifuge to isolate and concentrate the platelets, and then this "liquid gold" is injected back into your scalp.
Think of it as deploying a specialized repair crew right where it's needed most—your struggling follicles. These concentrated platelets are loaded with growth factors that help quell inflammation, trigger cell regeneration, and wake up dormant follicles, nudging them back into the growth phase. It’s a brilliant way to use your body's own healing power to revive your hair from the inside out, offering a promising and effective path forward for many different types of hair loss.
Your Top Scalp Health Questions, Answered
Living with a sensitive scalp day in and day out naturally brings up a lot of questions. When you're trying to figure out a scalp condition that's causing hair loss, you need practical advice, not just theories. Let's tackle some of the most common concerns to help you get a better handle on your scalp health.
Can Stress Really Make My Scalp Condition Worse?
Without a doubt, yes. Think of stress as fuel for inflammation. When you're under intense pressure, your body pumps out hormones like cortisol, which can kick inflammation into high gear all over your body—and your scalp is no exception.
This hormonal surge is often what triggers flare-ups of conditions like psoriasis and seborrheic dermatitis, making the itching and flaking feel a lot more severe. In more extreme cases, high stress can even lead to telogen effluvium, a condition where a shocking amount of hair suddenly shifts into the shedding phase all at once. Getting a handle on your stress is a massive step toward keeping your scalp calm and stable.
How Often Should I Actually Be Washing My Hair?
There's a stubborn myth floating around that washing your hair less will somehow "train" your scalp to be less oily. When it comes to inflammatory scalp conditions, that's usually the worst thing you can do.
In reality, letting oil, dead skin, and yeast build up is what really aggravates the irritation and inflammation. Washing more often—sometimes even daily—with the right gentle or medicated shampoo is key to clearing away that buildup. This one simple change can soothe inflammation and create a healthier environment where your hair follicles can thrive. It's always a good idea to ask a dermatologist what frequency is best for your specific situation.
A clean scalp is a calm scalp. Don't shy away from washing your hair as often as you need to. Keeping oil and flakes under control directly reduces the inflammation that can lead to hair shedding.
Are Natural Hair Products a Safer Bet for My Scalp?
Not always. "Natural" and "organic" are marketing terms, not medical ones. They don't guarantee a product will soothe your scalp or be free from irritants. While some plant-based ingredients are fantastic, others, like certain essential oils, are surprisingly common allergens.
Introducing an allergen to an already-inflamed scalp can easily make your condition worse. Instead of just looking for "natural" labels, you're better off seeking out products with proven active ingredients designed for your condition. Even better, look for products clearly labeled "fragrance-free" and "hypoallergenic" to minimize your risk of a bad reaction.
Here at PRP For HairLoss, we know that good information is the first step toward finding a solution. When you understand what’s causing your hair loss, you’re empowered to take back control of your scalp health. Take a look through our resources to learn more about advanced options like PRP therapy.
Find out more at https://prpforhairloss.com.

Leave a comment