If you've ever found yourself fighting with stubborn, flaky skin that just won’t give up, you might be dealing with seborrheic dermatitis. It’s a super common skin issue, basically a much more intense and stubborn version of dandruff.
And while a lot of people think of it as a scalp problem, this condition can pop up on any oily area of your body.
What Is Seborrheic Dermatitis?
Seborrheic dermatitis is a chronic inflammatory skin condition that causes red skin and flaky, yellowish scales. It’s important to get one thing straight right away: this condition is not contagious and isn’t a sign of poor hygiene. It's just your skin having an over-the-top reaction to a common microbe that lives on it.
This condition tends to appear where your oil-producing (sebaceous) glands are most active. Think of it as a communication breakdown—your skin's immune system gets irritated, leading to the inflammation, redness, and flaking that define a flare-up.
For a quick overview, here are the main things you'll see with this condition.
Seborrheic Dermatitis at a Glance
| Characteristic | Description |
|---|---|
| Appearance | Red skin covered with greasy scales or flakes. Can be yellowish or white. |
| Sensation | Often itchy, can sometimes feel like a slight burning sensation. |
| Common Areas | Scalp, face (eyebrows, sides of nose), ears, chest, and body folds. |
| Nature | Chronic, meaning it can have periods of flare-ups and remission. |
| Key Cause | An inflammatory reaction to Malassezia yeast, a normal inhabitant of the skin. |
While that table gives you the basics, let's take a closer look at where you're most likely to see it.
Common Hotspots for Flare-Ups
The scalp is ground zero for seborrheic dermatitis, but it’s definitely not the only spot. These flare-ups almost always happen in areas rich with oil glands.
- On the scalp: This is the classic presentation, what many people call severe dandruff.
- Around the face: You might notice it in your eyebrows, along the sides of your nose, or even behind your ears.
- On the chest: The middle of the chest, right between the pectoral muscles, is another frequent site.
- In body folds: Skin-on-skin areas like the armpits and groin can also be affected.
So, what’s really going on here? While experts haven’t nailed down a single cause, it’s widely believed to be a mix of factors. The main culprit is often an overgrowth of a naturally occurring skin yeast called Malassezia. For some folks, the immune system overreacts to this yeast, which triggers inflammation. Your genetics and hormones also have a big say in whether you're prone to it.
Key Takeaway: Seborrheic dermatitis is an inflammatory response, not an infection or a hygiene problem. It's a chronic condition, which means it can come and go. The goal is to manage the symptoms and keep those flare-ups to a minimum.
The inflammation itself can be a major issue, especially on the scalp. To dive deeper into this, you can explore the connection between scalp inflammation and potential hair loss in our dedicated guide.
How to Recognize the Symptoms
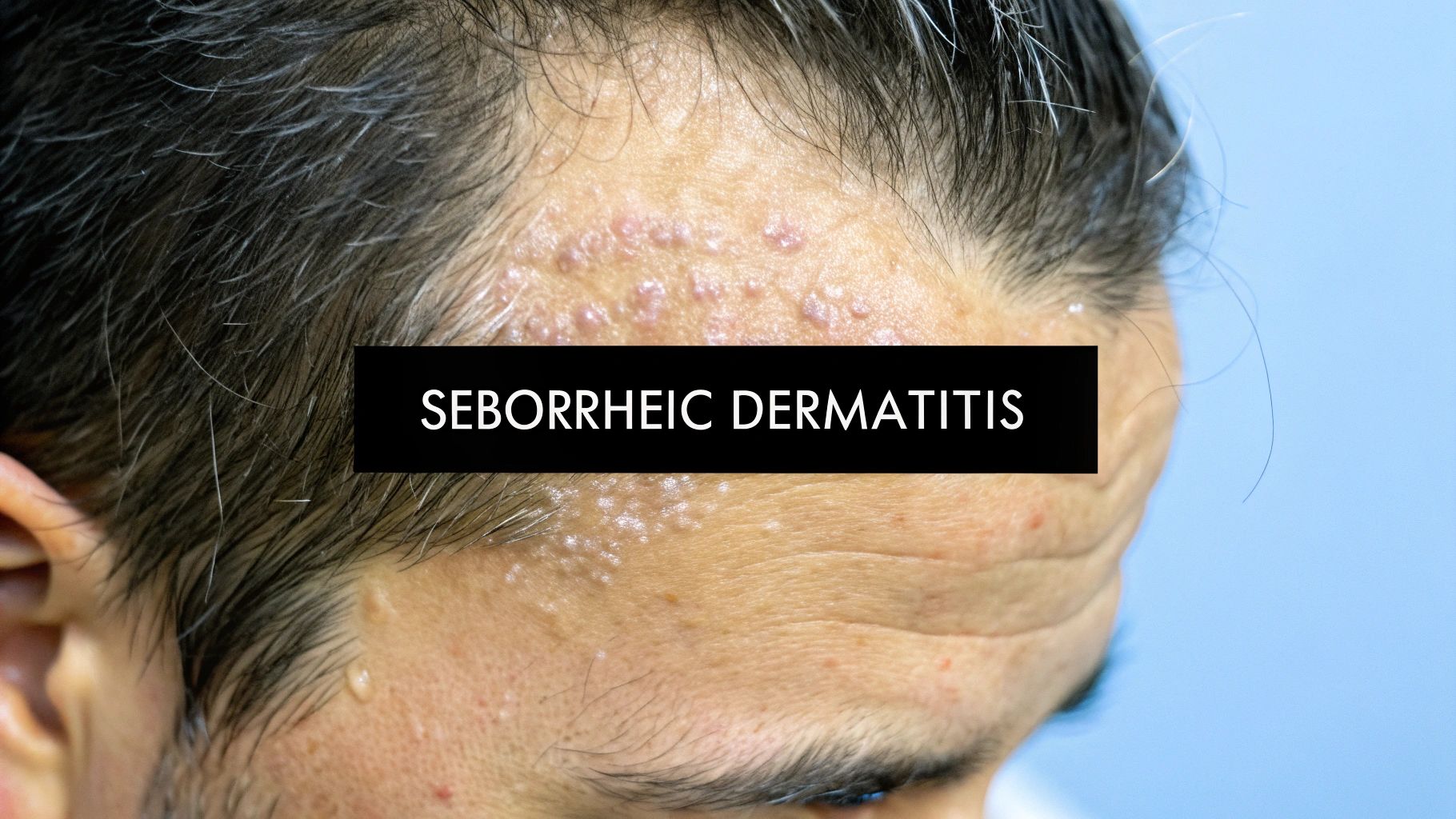
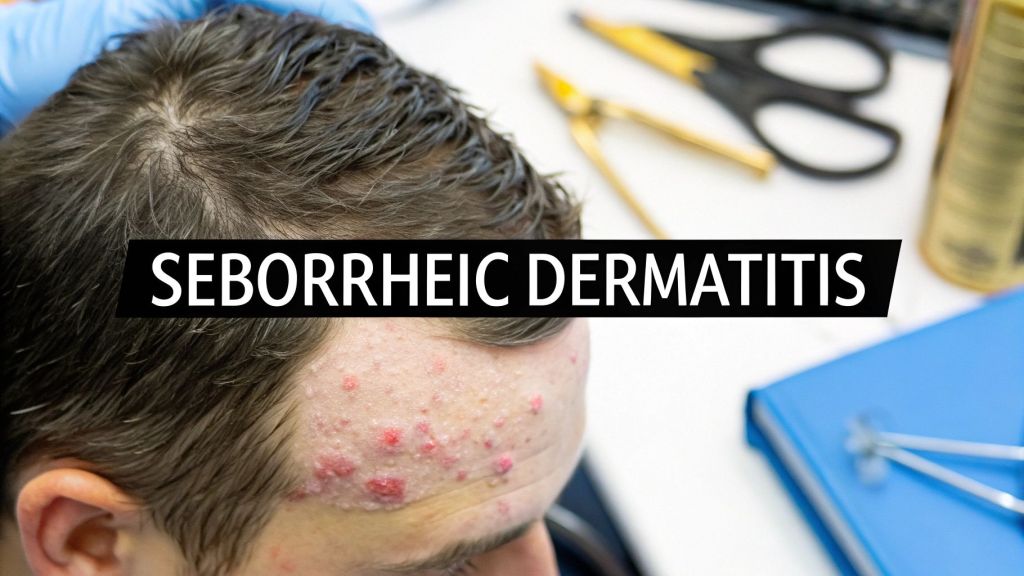
Figuring out if you have seborrheic dermatitis really comes down to spotting the specific signs, because it can easily be mistaken for simple dandruff or even just dry skin. The biggest giveaway is the kind of flakes you see. We're not talking about the fine, white dust of a dry scalp; these flakes are often yellowish or white and feel greasy or oily to the touch.
These scales don't just appear on their own—they sit on top of patches of red, inflamed skin. It's this one-two punch of greasy flakes and underlying redness that really points toward seborrheic dermatitis. On top of that, there's the itch, which can be anything from a minor annoyance to something that completely distracts you all day.
Where Symptoms Appear on the Body
While most people immediately think of the scalp, this condition loves to show up anywhere your skin is oily. The symptoms can look and feel a bit different depending on where they are.
- Scalp: This is the classic, stubborn "dandruff" that just won't quit. You’ll find greasy flakes in your hair and on your shoulders, along with a scalp that feels itchy and looks red.
- Face: It’s incredibly common for flare-ups to happen around the sides of the nose, in the eyebrows, on the eyelids, and even behind the ears. In these spots, the skin gets red and flaky.
- Chest and Body Folds: The middle of the chest, under the arms, and in the groin area are also prime real estate for these red, scaly patches because there's a higher concentration of oil glands.
In babies, this condition goes by a much gentler name: "cradle cap." It shows up as thick, crusty yellow or brown scales on the scalp. It might look a little alarming, but it’s usually not itchy or uncomfortable for the little one and typically clears up on its own.
Distinguishing It From Other Conditions
It’s easy to get skin conditions mixed up. For instance, psoriasis also causes red patches with scales, but those scales are usually much thicker, drier, and have a distinct silvery sheen. Eczema (atopic dermatitis), on the other hand, tends to hang out in the crooks of elbows and knees and is known for intensely dry, itchy skin, not greasy scales.
The hallmark of seborrheic dermatitis is the combination of greasy, yellowish scales on top of inflamed, red skin, primarily in oil-rich areas. Understanding this distinction is the first step toward finding the right way to manage it.
Think of this as a visual guide to help you connect the dots. Instead of just seeing "dry skin," you might now notice the flaking is specifically around your nose and eyebrows. Or that what you thought was just "bad dandruff" actually comes with a red, irritated scalp. Recognizing these specific patterns is the key to understanding what seborrheic dermatitis is and getting on the path to managing it effectively.
Uncovering the Root Causes and Triggers

If you're asking yourself why seborrheic dermatitis is happening, you're not alone. The frustrating truth is that it doesn’t come from one single thing you can easily point to. It’s more like a perfect storm where your body's internal workings and the world around you collide, sparking an inflammatory reaction on your skin.
Right off the bat, let's clear up a common misconception: this condition has nothing to do with poor hygiene. You could scrub your scalp raw and it wouldn't stop a flare-up. The problem isn't a lack of cleanliness; it's an internal response that’s largely out of your control.
The main suspect that researchers keep coming back to is a microscopic yeast called Malassezia. This tiny fungus lives on the skin of most adults without causing any trouble. But for people with seborrheic dermatitis, something goes haywire. The yeast might start to overgrow, and the immune system seems to overreact to it, launching an attack that results in the redness and flaking we see.
The Role of Malassezia Yeast
Think of your skin as a tiny, balanced ecosystem. When that balance gets thrown off—say, by an overproduction of your skin’s natural oil, called sebum—it creates the perfect five-star resort for Malassezia to multiply. Your immune system spots this party happening and, mistaking it for a threat, sounds the alarm. That inflammatory response is what you see and feel as a flare-up.
And this isn't some rare, obscure issue. A massive recent analysis found that about 4.38% of people worldwide are dealing with this, a number much higher than anyone thought. The research, which pooled data from over 1.26 million individuals, confirmed it's most common in adults. You can discover more insights about these global prevalence findings and see how the numbers look across different age groups.
Of course, the yeast is only part of the puzzle. Several other factors can make you more prone to a flare-up and influence just how bad it gets.
Key Contributing Triggers
A handful of other elements can pave the way for seborrheic dermatitis or make an existing case much worse. Getting a handle on these triggers is your first real step toward managing the symptoms.
- Genetic Predisposition: It often runs in families. If your parents or siblings have it, your odds of getting it are higher. This suggests some people are just genetically wired to have more reactive skin.
- Hormonal Fluctuations: Hormones are major players in oil production. It's no coincidence that flare-ups often appear during puberty, periods of high stress, or other times of significant hormonal shifts.
- Stress Levels: You're not imagining it—stress absolutely makes it worse. When you're stressed out, your immune system can go haywire, and your body's inflammatory response gets cranked up, leading to more frequent and stubborn flares.
- Environmental Factors: The weather can be a big trigger. Cold, dry air can suck the moisture out of your skin, while some people find that very humid conditions also aggravate their symptoms.
The Takeaway: Seborrheic dermatitis is a complex reaction shaped by your genes, immune system, hormones, and environment. It's not your fault. Pinpointing what triggers your flare-ups is the most powerful move you can make toward getting it under control.
Getting a Professional Diagnosis
https://www.youtube.com/embed/SwnWqOM79wE
If you’ve been looking at your skin and wondering if those flaky, red patches are really seborrheic dermatitis, your next move should be seeing a professional. The great news is that getting a diagnosis is usually pretty straightforward and doesn't involve a battery of complex tests.
Most of the time, an experienced dermatologist can identify the condition just by taking a close look at your skin.
They'll do a physical exam of the affected areas—your scalp, face, chest, or wherever you're having issues—and ask you about your experience. Be ready to talk about when the flare-ups began, how often they happen, and what you’ve noticed that makes them better or worse. This chat is a crucial piece of the diagnostic puzzle.
In the vast majority of cases, this visual check and conversation are all it takes to get a clear answer. But skin conditions can be tricky and sometimes look very much alike.
When Further Testing Is Needed
Every so often, your dermatologist might want to be 100% sure they aren't missing something. If your symptoms look a lot like other conditions such as psoriasis, eczema, or even a different type of fungal infection, they might suggest a skin biopsy.
A biopsy sounds way scarier than it actually is. It’s a very quick procedure where a tiny sample of skin is removed and sent to a lab to be examined under a microscope.
This gives a specialist a peek at what’s happening on a cellular level, which can provide a rock-solid, definitive diagnosis. It’s simply a way to rule out other possibilities and make sure your treatment plan is aimed at the right target.
A professional diagnosis is the foundation of an effective treatment strategy. It removes the guesswork, ensuring that the products and routines you use are right for your specific condition, not someone else's.
If the issue is on your head and you're curious about the procedure, learning more about a scalp biopsy for hair loss can give you a better idea of what to expect. Getting a firm diagnosis is the first real step toward taking control and starting a treatment that finally brings you relief.
Finding an Effective Treatment Plan
Trying to find the right treatment for seborrheic dermatitis can feel like you're staring at a huge wall of options. The good news is that for most people, the journey to relief starts with a simple trip to the pharmacy. Over-the-counter (OTC) products are the first line of defense, and they’re designed to tackle the two main culprits: yeast overgrowth and inflammation.
It helps to think of these treatments as your personal toolkit. You won't need every tool for every flare-up, but knowing what's available means you can grab the right one when you need it. Sticking with a routine is absolutely key, but don't be surprised if you have to switch things up now and then to keep your scalp responding well.
The image below breaks down a basic three-step routine that can serve as the backbone of your management plan.
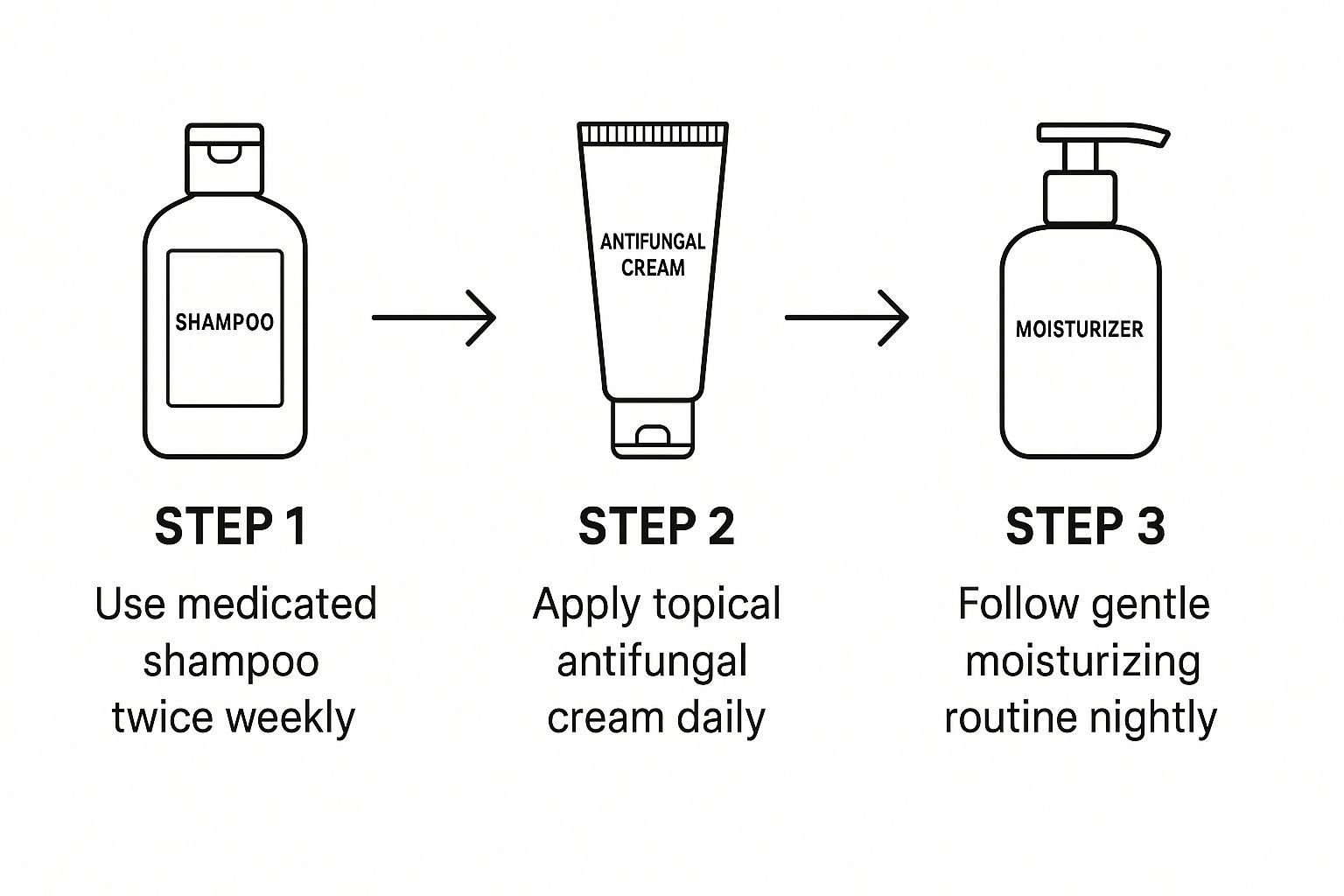
As you can see, a combination of medicated shampoos, specific topicals, and gentle moisturizers works together to create a solid daily and weekly care system.
Over-The-Counter Solutions
When you start looking at OTC shampoos, you'll quickly notice a few active ingredients that show up all the time. Each one has a slightly different job, but they all work toward bringing your scalp back to a healthy state.
- Zinc Pyrithione: This is a popular antifungal and antibacterial agent that helps get the Malassezia yeast population under control.
- Selenium Sulfide: This ingredient does two things—it slows down how quickly your skin cells turn over and it has antifungal properties.
- Ketoconazole: A straight-up powerful antifungal, this one directly fights the yeast overgrowth driving your flare-ups. We dive deeper into its benefits in our guide on ketoconazole shampoo.
- Coal Tar: An old-school but effective remedy, coal tar works by slowing down skin cell growth on the scalp, which in turn reduces scaling and inflammation.
Here's a pro tip: try rotating between two different types of medicated shampoos. Using one for a few weeks and then swapping it for another can prevent the yeast from building resistance, keeping the treatments effective over the long haul.
Finding your perfect combination is often a matter of trial and error. What's a miracle product for one person might do very little for you, so give yourself some grace as you figure out what your skin prefers.
When to Consider Prescription Treatments
If you’ve been diligently using OTC products for several weeks and you're just not seeing results, it’s probably time to see a doctor. They have access to prescription-strength options that can deliver a much stronger punch. These might include more potent antifungal creams or a short course of topical corticosteroids to knock down severe redness and itching fast.
And this isn't an isolated problem. The annual number of new seborrheic dermatitis cases worldwide hit approximately 135.7 million in 2021, which is a massive increase from the 88.5 million cases back in 1990. This rise in diagnoses highlights just how important it is to know all your treatment options.
While seborrheic dermatitis is its own unique condition, looking at how other inflammatory skin issues are managed can be helpful. For instance, learning about rosacea treatments that calm redness can provide some useful parallels for soothing irritated skin. At the end of the day, a smart mix of consistent at-home care and professional medical advice is your best strategy for keeping those frustrating symptoms in check.
Lifestyle Changes for Long-Term Management

While medicated shampoos and creams are fantastic for knocking down a flare-up, they're only part of the solution. If you really want to manage seborrheic dermatitis for the long haul, you need to look at your daily habits.
Think of it like this: treatments are the firefighters putting out the blaze, but lifestyle changes are the fire prevention plan. By making a few smart adjustments, you can significantly cut down on how often and how severely you experience symptoms, giving you back control.
Gentle Skin and Scalp Care
One of the simplest yet most effective changes you can make is to just be kinder to your skin. Aggressive scrubbing and harsh soaps do more harm than good, stripping away your skin’s natural defenses and making inflammation even worse.
The key is consistency with a gentle routine. It’s not about doing more; it’s about doing the right things day in and day out.
- Pick the Right Cleansers: Switch to gentle, non-soap cleansers for your face and body. Check the label for products that are alcohol-free and designed for sensitive skin.
- Moisturize Every Day: Don't skip this, even if your skin feels oily. A light, non-comedogenic moisturizer helps keep your skin barrier strong and resilient.
- Turn Down the Heat: Super hot showers feel great, but they strip your skin of its protective oils. Stick with lukewarm water to keep irritation at bay.
For guys dealing with scalp issues in particular, a dedicated routine can be a game-changer. Our guide to men's scalp care has some targeted advice that builds on these tips.
The Mind-Body Connection
Your skin is often a billboard for what’s happening on the inside. Things like stress, sleep, and what you eat have a direct impact on inflammation, which is the root cause of seborrheic dermatitis.
Stress is a huge, well-known trigger for flare-ups. When you're stressed, your body pumps out hormones that crank up oil production and inflammation—the perfect storm for a breakout.
This is where stress management becomes skin management. Finding what works for you, whether it's exercise, meditation, or just taking five-minute breaks, can make a real difference. Likewise, getting a solid 7-9 hours of quality sleep gives your body the downtime it needs to repair and keep its immune system in check. A balanced, anti-inflammatory diet also goes a long way in giving your skin the nutrients it needs to thrive.
Common Questions About Seborrheic Dermatitis
Even with a good handle on the basics, you probably still have some nagging questions. That’s completely normal. Living with seborrheic dermatitis brings up a lot of practical, day-to-day uncertainties. Getting clear on these can make all the difference in managing your skin with confidence.
Let's dive into some of the questions I hear most often to give you the full picture.
Is Seborrheic Dermatitis the Same as Dandruff?
Not quite, but they're definitely related. It helps to think of dandruff as the very mildest form of seborrheic dermatitis—one that’s confined to the scalp and doesn't involve any real inflammation.
Once you start seeing redness, greasy-looking scales, and noticeable irritation, and it spreads to places like your face or chest, you’ve crossed the line into what we officially call seborrheic dermatitis.
Can It Be Permanently Cured?
Unfortunately, there's no permanent cure right now. Seborrheic dermatitis is a chronic condition, which means it’s something you manage for the long term. It will likely have periods where it flares up and times when it’s much calmer.
But that absolutely doesn’t mean you can't find relief. With a consistent treatment plan and some smart lifestyle changes, you can keep symptoms under control and enjoy long stretches of clear, comfortable skin.
The goal isn't a one-and-done fix; it's about finding a sustainable management strategy. The real key is learning your personal triggers and sticking to a routine that keeps your skin happy.
Does Diet Really Affect Flare-Ups?
While researchers are still working to pin down the exact scientific connection, a lot of people report a clear link between what they eat and how their skin behaves. It's a very common anecdotal finding. Many find that pro-inflammatory foods—things like sugar, dairy, and highly processed carbs—tend to make their symptoms much worse.
On the flip side, adopting an anti-inflammatory diet full of leafy greens, berries, and omega-3-rich fish might help calm your skin down. A great way to figure out what affects you is by keeping a simple food diary to identify your own personal dietary triggers.
The prevalence of this condition varies wildly across the globe. One large analysis combining 121 different studies found a global average of 4.38%, but in certain clinical settings, that rate has been reported as high as 30.03%. You can discover more about how prevalence differs by setting and population. If your symptoms just won't quit despite your best efforts, knowing when to see a dermatologist is the most critical next step.
At PRP For HairLoss, we're committed to providing clear, reliable information on scalp health and hair loss solutions. Explore our resources to find the answers you need: https://prpforhairloss.com
Leave a comment