When you hear "hair loss," you probably think of common conditions like male pattern baldness or alopecia areata. But there's another, less common category of hair loss that’s in a league of its own: scarring alopecia, also known as cicatricial alopecia.
This isn't just about hair falling out. It's about the hair follicle itself being permanently destroyed by inflammation.
What Is Scarring Alopecia and How Is It Different?
Think of your scalp as a garden. In typical hair loss, the plants (your hair) might wither or fall out, but the soil—the follicle—is still viable, ready to grow new hair.
With scarring alopecia, the soil itself is the problem. Inflammation attacks and destroys the hair follicle, and the body rushes in to replace it with scar tissue. Once that scar tissue forms, the ground is no longer fertile. No new hair can ever grow from that spot again.
This permanence is what truly sets scarring alopecia apart. It’s not just one disease, but a whole collection of disorders that all share this destructive outcome. Getting your head around this key difference is the first step in tackling the condition.
The Mechanism of Permanent Hair Loss
The road to permanent hair loss in scarring alopecia is a destructive cycle fueled by inflammation. It usually unfolds in three stages:
- Inflammation Begins: For reasons that aren't always clear, inflammatory cells get the wrong signal and start to attack the hair follicles.
- Follicle Destruction: This relentless inflammation damages the vital stem cells in the follicle that are responsible for hair regeneration. Once they're gone, the follicle can't rebuild itself. To get a deeper look at this process, you can read about how hair follicles die and what it means for regrowth.
- Scar Tissue Formation: The body's natural healing response kicks in, filling the void left by the destroyed follicle with fibrous scar tissue. This essentially paves over the "soil," sealing the deal on permanent hair loss in that area.
This infographic gives a great visual breakdown of how this destructive process works.
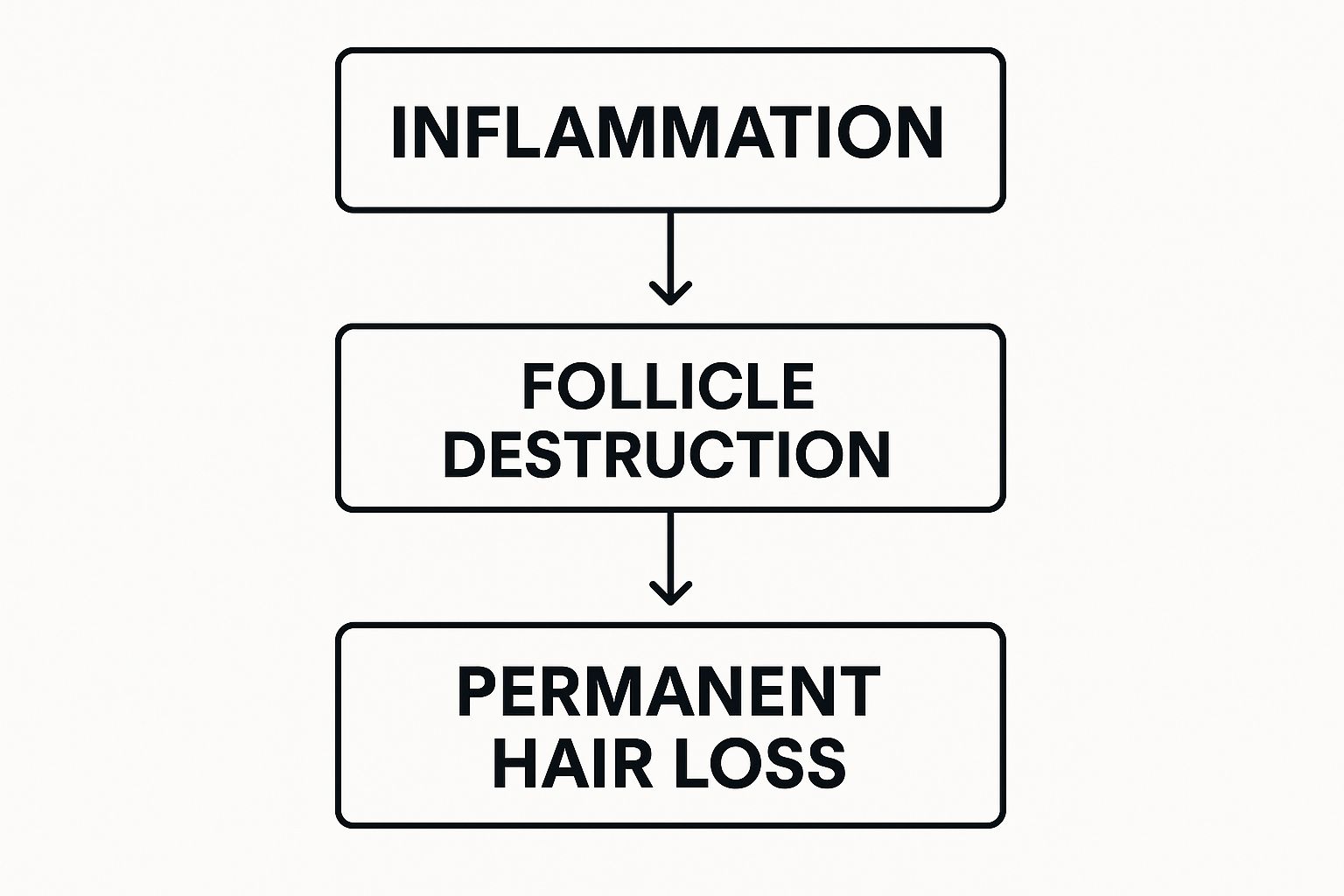
As you can see, the inflammation is the real culprit that leads directly to follicle destruction and, ultimately, the scarring that prevents regrowth.
While not as common as other forms of hair loss, its impact is often more severe because it's permanent. The primary goal of any treatment is to shut down this inflammatory process before more follicles are lost for good.
Though it might feel like a rare condition, scarring alopecias are more common than you might think. One multicenter study revealed they make up about 27% of all alopecia diagnoses globally. This really highlights how critical it is to get an early, accurate diagnosis to save the hair you still have.
Scarring vs Non-Scarring Alopecia: Key Differences
To help you grasp the fundamental differences between these two main categories of hair loss, here’s a quick summary.
| Feature | Scarring Alopecia (Cicatricial) | Non-Scarring Alopecia (e.g., Alopecia Areata) |
|---|---|---|
| Follicle Status | Destroyed and replaced by scar tissue | Preserved, but dormant or miniaturized |
| Hair Regrowth | Not possible in scarred areas | Often possible with or without treatment |
| Primary Cause | Inflammation directly targeting the hair follicle | Various (autoimmune, hormonal, genetic) |
| Scalp Appearance | Can show redness, scaling, pustules, or smooth skin | Usually appears normal, without visible scarring |
| Treatment Goal | Stop inflammation and prevent further hair loss | Stimulate hair regrowth |
This table makes it clear: with scarring alopecia, the fight is to preserve what's left, while with non-scarring types, the focus is all about encouraging regrowth.
Navigating the Different Types of Scarring Alopecia
It’s easy to think of scarring alopecia as a single condition, but it's really an umbrella term for a whole group of different disorders. Getting a handle on these distinctions is the first real step toward understanding a diagnosis and finding a path forward.
These types are usually sorted by which inflammatory cells are leading the charge against the hair follicles. This might sound a little technical, but think of it like identifying pests in a garden. You wouldn't use the same treatment for aphids as you would for slugs, right? It's the same idea here—pinpointing the exact type of inflammatory cell helps us choose the most effective strategy to protect your scalp.
The two main groups we see are lymphocytic and neutrophilic alopecias.
Lymphocytic Alopecias: When the Body's Defenses Go Awry
In the lymphocytic forms of scarring alopecia, the aggressors are lymphocytes—a type of white blood cell that’s part of your immune system. For reasons we’re still piecing together, these cells mistakenly flag hair follicles as a threat.
It’s essentially a case of friendly fire. The body’s own defense system turns on itself, sparking inflammation that ultimately destroys the follicle.
Some of the most common types in this group include:
- Lichen Planopilaris (LPP): This one often shows up as tiny, reddish-purple bumps around hair follicles, usually on the crown or top of the head. People with LPP frequently experience intense itching, tenderness, and a burning sensation, which gives way to smooth, scarred patches where hair no longer grows.
- Frontal Fibrosing Alopecia (FFA): Often considered a variant of LPP, FFA is known for its distinct pattern. It creates a slow but steady band of hair loss that moves back from the frontal hairline. Eyebrows are often affected, too. The skin in the area typically looks pale and unusually smooth.
- Central Centrifugal Cicatricial Alopecia (CCCA): As the name hints, this condition usually starts at the center of the scalp (the crown) and spreads outward in a circular pattern. It is most commonly seen in women of African descent and is thought to have links to both genetic predispositions and certain long-term hair care practices.
With these conditions, the main goal of treatment is to calm down the overactive immune response and put a stop to the inflammation.
Neutrophilic Alopecias: The Infection Responders
The second category is neutrophilic scarring alopecia. Here, the primary cells causing the trouble are neutrophils. This type often looks more like a chronic infection, with pustules and pus-filled bumps on the scalp, and can be triggered by the body's reaction to bacteria or other microbes.
The two main examples here are:
- Folliculitis Decalvans: This condition is marked by recurring pimple-like pustules and crusting that lead to expanding patches of scarred hair loss. It can be quite painful and often feels like a scalp infection that just won't go away.
- Dissecting Cellulitis of the Scalp: This is a rarer and often more severe condition. It involves deep, painful abscesses and interconnected tunnels (sinus tracts) forming under the scalp. As these areas heal, they leave behind significant, bumpy scars.
While the names sound complex, the key takeaway is simple: the type of scarring alopecia dictates the symptoms you might experience and the treatment path a specialist will recommend.
Among all these subtypes, some pop up more frequently than others. Research shows that frontal fibrosing alopecia is the most frequent subtype, making up about 10.8% of all cases, followed closely by lichen planopilaris at 7.6%.
These conditions are seen most often in women, especially as they get older. You can learn more about the prevalence of these conditions from recent studies. This data really drives home why it's so crucial for specialists to recognize the specific patterns of hair loss to land on the right diagnosis.
Exploring the Causes and Risk Factors
When you’re dealing with something as personal as hair loss, the first question is almost always, "Why is this happening to me?" With scarring alopecia, the answer isn't so simple. It’s not about one single thing going wrong; it's more like a perfect storm where the body's defense systems mistakenly turn against the hair follicles.
At its core, scarring alopecia is driven by an out-of-control inflammatory response. Imagine your immune system as a security team that’s supposed to protect you from germs and viruses. In this case, it gets its wires crossed and misidentifies your hair follicles as a threat. This triggers a relentless attack that, over time, causes so much damage that the follicle is permanently destroyed. We don't always know the exact trigger, but we've pieced together some of the most common culprits.
The Interplay of Internal and External Triggers
Figuring out what kicks off this inflammation is the key to understanding the condition. The causes can usually be traced back to a few main areas, and often, it’s a combination of factors working together.
Here are some of the primary drivers we see behind scarring alopecia:
- Autoimmune Responses: In conditions like Lichen Planopilaris, the immune system directly targets healthy hair follicles. This is a classic case of friendly fire and one of the most frequent reasons for this kind of permanent hair loss.
- Genetic Predisposition: Sometimes, your DNA just makes you more vulnerable. For instance, Central Centrifugal Cicatricial Alopecia (CCCA) is most common in women of African descent, pointing to a strong genetic link that other factors can then activate.
- Chronic Infections: A stubborn bacterial or fungal infection can sometimes provoke such a fierce and prolonged inflammatory reaction that it ends up destroying the follicles. Folliculitis Decalvans is a perfect example of this process in action.
- Physical Trauma or Stress: It's not just internal issues. Repeated physical stress on your hair follicles—from years of tight hairstyles or harsh chemical treatments—can also set off this destructive inflammatory cycle.
While each of these pathways is different, they all lead to the same unfortunate place: inflammation that permanently wipes out the hair follicle. This is fundamentally different from more typical hair thinning. To get a broader perspective, you can learn more about the general causes of hair loss and see how they differ.
Who Is Most Commonly Affected?
Scarring alopecia can technically affect anyone, but certain types definitely have their preferences. Demographics like age, gender, and ethnicity can be major risk factors, giving us valuable clues when it comes to diagnosis.
A classic example is Frontal Fibrosing Alopecia (FFA). This condition almost exclusively affects postmenopausal women, creating a very distinct receding hairline at the front of the scalp. Spotting these trends allows specialists to connect the dots and reach a diagnosis much faster.
This doesn't mean men or younger women are completely in the clear, but it shows how powerful things like hormonal shifts and age can be as triggers. Ultimately, getting to the root of scarring alopecia is all about understanding the delicate systems at play in your body and figuring out what might have thrown them off balance.
Recognizing Early Symptoms and Warning Signs

When it comes to scarring alopecia, catching it early isn't just a good idea—it's everything. The damage is permanent, so the entire goal is to step in before the hair loss becomes widespread. This means learning to spot the subtle clues your scalp is sending, often long before you notice any significant thinning.
The earliest signs are usually flags for active inflammation, the very process that's attacking and destroying your hair follicles. While most people think of hair loss as seeing more strands in the shower, the first warnings for this condition are often felt rather than seen.
Beyond Hair Thinning: What to Look For
The initial signs of scarring alopecia are rarely about shedding. They're physical sensations on your scalp that point to that underlying inflammatory attack. If you're experiencing any of the following, your body might be telling you something is wrong.
Watch out for these common early symptoms:
- Persistent Itching: This isn't just a random itch. It's a nagging, constant sensation that won't go away, often focused on specific spots.
- Burning or Pain: Many people describe a distinct burning feeling or a tender, sore scalp that’s painful to the touch.
- Visible Redness: The skin in the affected areas of your scalp may look pink, red, or generally inflamed.
- Pustules or Bumps: You might see small, pimple-like bumps—sometimes filled with pus—popping up around your hair follicles.
- Scaliness or Flaking: You may notice flaky skin or crusting around the base of your hairs, almost like a severe form of dandruff.
These symptoms are your body’s alarm bells, signaling that your follicles are in trouble. If you’re trying to determine what’s normal, it helps to understand how to tell if your hair is thinning versus showing these signs of inflammation.
Don't dismiss persistent scalp discomfort as a minor issue. In scarring alopecia, symptoms like itching and burning are the frontline indicators of active follicle destruction. Acting on them quickly can make all the difference.
The Importance of Early Detection
Because the hair loss is irreversible, time is not on your side. While it's tough to get exact numbers, some studies from specialized clinics suggest that up to 27% of patients presenting with hair loss have some form of scarring alopecia. The stakes are higher than with non-scarring types, as it often comes with distressing symptoms like the itching and burning mentioned above. You can discover more insights about these findings in related population studies.
Recognizing the early symptoms is your best defense. If you notice any of these warning signs, the most critical next step is getting a professional diagnosis from a dermatologist. Early intervention gives you the best possible chance to halt the inflammation, stop the disease from progressing, and save the hair you still have.
How Scarring Alopecia Is Professionally Diagnosed
https://www.youtube.com/embed/pPU1E6RfhQA
Getting the right diagnosis is, without a doubt, the most critical step in tackling scarring alopecia. The whole game is about stopping the inflammation before it destroys more hair follicles for good, so you can't afford to guess.
The process usually starts with a detailed chat and a close look at your scalp by a dermatologist. They’re trained to spot the subtle (and sometimes not-so-subtle) signs of trouble like redness, scaling, or pustules around the hair follicles. They’ll also dive into your personal and family medical history to connect the dots.
Getting a Closer Look with Trichoscopy
To get a much better view of what’s happening, your doctor will likely use a special handheld magnifying tool called a dermatoscope. This technique, called trichoscopy, lets them see your scalp and hair follicles up close and personal, without any need for a sample. It’s completely non-invasive.
Think of it like a detective using a high-powered magnifying glass. Trichoscopy helps the dermatologist see key clues that are invisible to the naked eye, such as:
- The loss of hair follicle openings (the little dots where hair should be).
- Unique patterns of scaling or redness right around the follicles.
- Changes in the tiny blood vessels supplying the scalp.
This close-up look gives them a much clearer picture of the inflammation and helps them pinpoint the best spot for the next step, which is often the deciding factor.
The Scalp Biopsy: The Gold Standard
While a visual exam and trichoscopy can point strongly in one direction, the definitive way to diagnose scarring alopecia is with a scalp biopsy. This straightforward procedure is done right in the office and provides the final piece of the puzzle.
A biopsy isn't just about confirming a diagnosis; it’s about understanding exactly what's happening under the skin. It reveals the inflammation, shows the scar tissue, and helps identify the precise type of scarring alopecia you're dealing with.
The procedure itself is quick. Your dermatologist numbs a small area of your scalp and takes a tiny skin sample, usually just 4mm wide, to send off to a lab. While the idea might sound a bit intimidating, learning about why a scalp biopsy for hair loss is so important can help put your mind at ease. This one small step is what ensures your treatment plan is built on a rock-solid diagnosis.
Current Treatment Approaches for Managing the Condition

Getting a scarring alopecia diagnosis can feel like a gut punch, but it’s crucial to know that you're not out of options. While we can’t turn back the clock on follicles that are already lost, the primary goal of treatment is crystal clear: to stop the inflammation and prevent the condition from getting worse.
Think of it like firefighters battling a blaze. The fire (inflammation) has unfortunately already damaged part of the forest (your hair follicles), but a skilled crew can create a firebreak to save the healthy trees that remain. That's exactly what we aim to do with scarring alopecia treatment—preserve the healthy, functioning follicles you still have.
There’s no cookie-cutter solution here. Instead, your dermatologist will craft a personalized strategy designed to get the specific type of inflammation driving your hair loss under control.
Medical Interventions to Control Inflammation
The first line of defense almost always involves medications that either calm the overactive immune response or, in some cases, fight off an underlying infection. These treatments are all about targeting the root cause of the follicle destruction.
The most common tools in our medical toolbox include:
- Topical Steroids: These are usually creams, foams, or lotions you apply directly to your scalp. They work on-site to reduce inflammation right at the source by suppressing the local immune activity.
- Corticosteroid Injections: For a more potent, targeted approach, a dermatologist can inject corticosteroids directly into the inflamed patches on the scalp. This gets the powerful anti-inflammatory medicine exactly where it’s needed most. You can learn more in our detailed guide on corticosteroids and hair loss.
- Oral Medications: When the condition is more aggressive or widespread, your doctor might prescribe pills. These could be anti-inflammatory drugs like hydroxychloroquine or even immunosuppressants designed to dial down your body's entire immune system. For conditions like folliculitis decalvans where bacteria are involved, antibiotics become a key part of the plan.
The name of the game with medical treatment is proactive management. The ultimate objective is to push the condition into remission, a quiet phase where the inflammation is no longer active and hair loss stops.
Supporting Therapies and Hair Health
Beyond the frontline medical treatments, many people look into supportive therapies to improve overall scalp health and create a better environment for their remaining hair. One complementary treatment often discussed in this context is Platelet-Rich Plasma (PRP) therapy.
PRP uses a concentration of your own blood platelets, which are packed with growth factors. The idea is to inject this "liquid gold" into the scalp to help support follicles that are inflamed but haven't been destroyed yet. While it isn't a cure, some see it as a way to help manage inflammation and nurture the surrounding tissue.
Alongside professional treatments, it's also about good daily care. Many people focus on finding the best hair growth products to gently maintain the hair they have.
Because the hair loss is permanent, catching it and starting treatment early is absolutely essential. Unfortunately, challenges exist because these are rare disorders, and their impact on a person's quality of life and mental well-being can be significant. You can learn more about these therapeutic challenges from ongoing research in the field. Ultimately, finding the right combination of treatments is a journey you'll take with your dermatologist, based on your specific diagnosis and how you respond.
Common Questions About Scarring Alopecia
Getting a diagnosis like scarring alopecia can leave you with a lot on your mind. It’s completely normal to have questions, and getting clear answers is the first step toward feeling more in control. Let's walk through some of the most common concerns we hear from patients.
Can Hair Grow Back with Scarring Alopecia?
This is often the first question people ask, and unfortunately, the answer is no. Once a hair follicle has been destroyed and replaced by scar tissue, the hair loss in that specific spot is permanent. The damage simply can't be undone.
The main goal of treatment, then, isn't regrowth in the scarred areas. Instead, we focus on halting the inflammation to prevent the condition from spreading. It's all about protecting the healthy follicles you still have and preserving your remaining hair.
Is This Condition Contagious?
Absolutely not. Scarring alopecia is not contagious. It’s an internal condition, usually driven by inflammation or an autoimmune response within your own body.
You can't catch it from someone else or pass it to them through touch, sharing a hat, or using the same hairbrush.
How Long Does Treatment for Scarring Alopecia Last?
There's no one-size-fits-all answer here; the duration of treatment really depends on the individual. It's influenced by the specific type of scarring alopecia you have, how aggressive it is, and how your body responds to the chosen therapy.
For many people, managing scarring alopecia is a long-term commitment. Think of it less as a "cure" and more as ongoing management. Consistent therapy is often necessary to keep inflammation in check, control symptoms, and prevent future flare-ups from causing more permanent hair loss.
At PRP For HairLoss, we're dedicated to providing clear, reliable information about hair loss conditions and innovative treatments. Learn more about how PRP therapy may fit into your hair health journey.

Leave a comment