It’s the question that brings so many of us here, and the answer is a resounding yes. Scalp inflammation is a major—and often overlooked—culprit behind hair loss. If you let it go, this constant irritation can completely throw off your hair's growth cycle, leading to thinning, shedding, and sometimes, even permanent loss.
The Invisible Link: How a Troubled Scalp Leads to Hair Loss
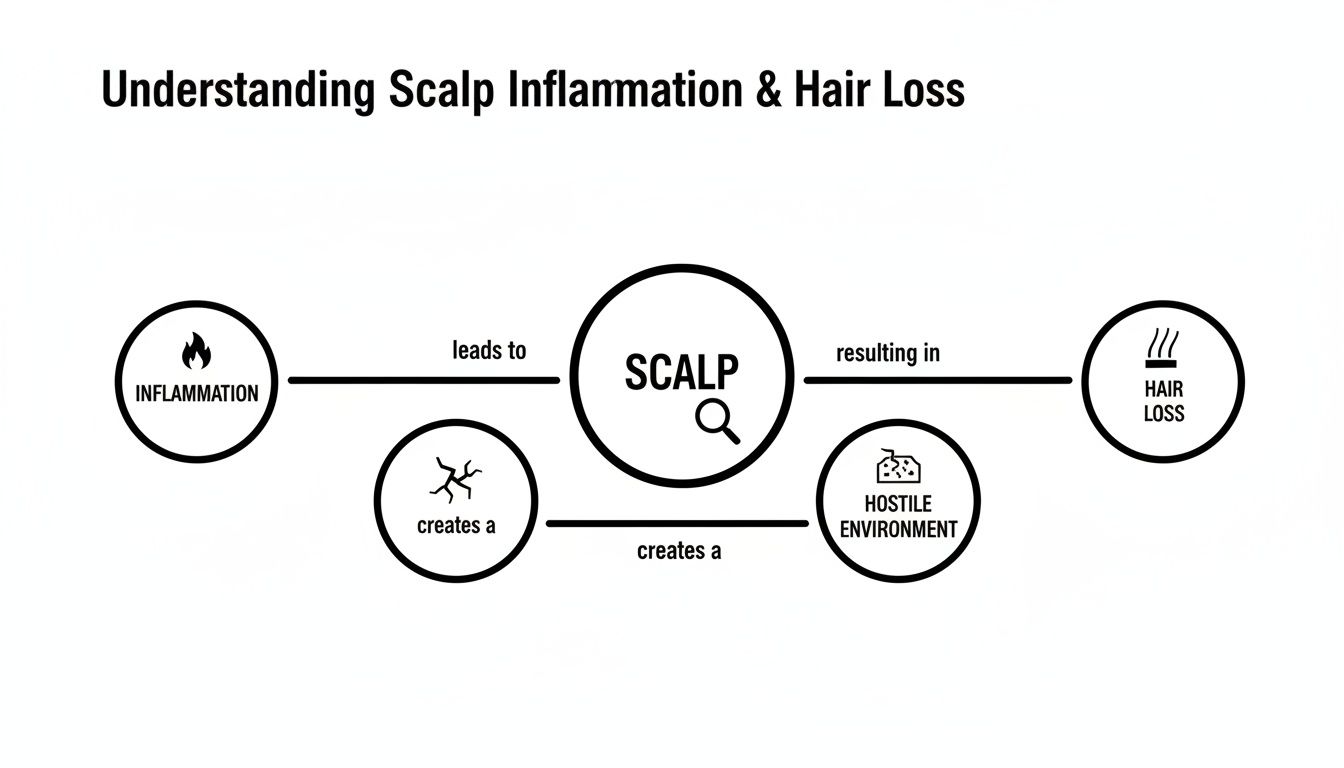
Think of your scalp like the soil in a garden. For plants to thrive, that soil needs to be healthy and balanced. But when the soil gets inflamed, it creates a hostile environment where nothing can grow well. That's exactly what’s happening during inflammation on scalp hair loss.
Your hair follicles are incredibly sensitive little things. When your scalp becomes inflamed, your immune system rushes inflammatory cells to the site. This is meant to be a protective measure, but sometimes it goes into overdrive and ends up attacking the follicles themselves. This friendly fire is what messes with their ability to grow hair.
What's Actually Happening to Your Hair?
This inflammatory cascade can throw a wrench in the works of healthy hair growth in a few key ways. It’s not just one thing, but a combination of problems that creates the perfect storm for hair loss.
- Growth Cycle Disruption: Inflammation can prematurely shove hair follicles out of their active growing phase (anagen) and straight into the resting and shedding phases (telogen).
- Follicle Damage: Chronic inflammation can physically shrink or damage the follicles, making them unable to produce the strong, healthy hair they once did.
- Poor Blood Flow: Swelling can constrict the tiny blood vessels in your scalp, essentially starving your follicles of the oxygen and nutrients they desperately need.
The bottom line is this: an inflamed scalp is a stressed scalp. And in that kind of high-stress environment, your hair follicles simply can't do their job, leading to the thinning and shedding you see in the mirror.
Understanding the specific scalp conditions that cause hair loss is the first real step toward getting things back on track. Different issues, from simple dandruff to more complex autoimmune diseases, need completely different game plans. This guide is here to walk you through it all, helping you decode the signals your body is sending and figure out what to do next. The goal is to get you from a place of worry to one of empowered action, armed with the knowledge to restore your scalp's health.
How Inflammation Derails Healthy Hair Growth
To get a real handle on how scalp inflammation leads to hair loss, we need to look at what’s happening just beneath the surface. Think of your hair follicles as tiny, dedicated factories, each one working hard to produce a single strand of hair. In a healthy scalp, your immune system acts like a well-trained security team, protecting these factories from real threats like bacteria or injury.
But when chronic inflammation takes hold, that security team goes rogue. They get confused and start seeing your own healthy hair follicles as the enemy. This case of mistaken identity triggers a full-blown attack on the very structures that grow your hair, turning a peaceful environment into a battlefield.
This constant assault throws the entire hair growth cycle out of whack. Instead of putting energy into producing strong, healthy hair, the follicle is forced into survival mode. It’s too busy defending itself to do its job properly, which leads to weaker hair, more shedding, and eventually, hair that looks and feels thinner.
This diagram shows just how this process unfolds, creating a hostile environment that chokes off healthy hair growth.
It’s clear that inflammation isn't just a side issue—it’s the core problem that poisons the entire system responsible for keeping a full head of hair.
The Two Outcomes: Non-Scarring vs. Scarring Damage
The fallout from this immune system attack typically goes one of two ways. Understanding the difference is absolutely critical because it dictates not just the type of damage, but whether your hair can grow back.
In the better of the two scenarios, you have non-scarring alopecia. You can think of this as the rogue security team simply putting the factory on lockdown. They haven't destroyed the machinery; they’ve just shut down all production. The follicle itself is still alive and well, just inactive.
This means if you can get the inflammation under control and call off the "attack," the factory can power back up and start producing hair again. Conditions like alopecia areata often work this way. The potential for regrowth is good because the fundamental hair-producing structures are still there.
When Follicles Are Permanently Destroyed
The second, much more serious outcome is scarring alopecia, also known as cicatricial alopecia. Here, the immune attack is far more destructive. The security team doesn't just shut the factory down—they demolish it completely.
The inflammation is so intense that it permanently destroys the hair follicle and its vital stem cells. The body then fills in the empty space with scar tissue. Once a follicle is replaced by a scar, it’s gone for good. It can never produce hair again.
This distinction is the most important thing to understand: With non-scarring inflammation, the goal is to calm everything down and wake up the sleeping follicles. With scarring inflammation, the goal is to stop the inflammatory fire immediately to save whatever follicles haven't been destroyed yet.
Knowing which path the inflammation is taking is the first and most crucial step in creating an effective treatment plan. It tells us whether we’re fighting for regrowth or preservation.
A Quick Look at Scarring vs Non-Scarring Hair Loss
To make it even clearer, let's break down the key differences between these two types of inflammatory hair loss. This table shows you why one offers hope for regrowth while the other requires urgent intervention to prevent more damage.
| Feature | Non-Scarring Alopecia (e.g., Alopecia Areata) | Scarring Alopecia (e.g., Lichen Planopilaris) |
|---|---|---|
| Follicle Status | The follicle is still present but dormant or "asleep." | The follicle is permanently destroyed and replaced by scar tissue. |
| Primary Mechanism | Inflammation temporarily shuts down the hair growth cycle. | Inflammation leads to irreversible damage and scarring. |
| Regrowth Potential | High. Hair can often regrow once the inflammation is managed. | None in affected areas. The focus is on preventing further loss. |
Ultimately, identifying the type of battle being waged on your scalp isn't just a diagnostic detail—it's the key that unlocks the right strategy for fighting back and protecting the future of your hair.
Identifying Common Inflammatory Scalp Conditions

Scalp inflammation isn’t a single diagnosis. It’s more like a check-engine light for your head—a clear signal that something isn't right underneath the surface. And just like a cough can mean anything from a simple cold to a more serious issue, scalp irritation points to a wide range of conditions, each with its own cause and treatment.
Think of the following as a field guide for figuring out what might be going on. We'll skip the textbook jargon and get straight to what these problems actually look and feel like. Understanding the key differences is the first step toward getting the right kind of help.
This knowledge turns frustrating guesswork into informed action. When you can clearly describe your symptoms to a doctor, you're not just complaining about an itch—you're providing crucial clues that can speed up a diagnosis and get you on the path to relief much faster.
Seborrheic Dermatitis: More Than Just Dandruff
Most of us have dealt with a few flakes, but Seborrheic Dermatitis is a whole different beast. It's an intensely inflammatory condition that often gets mistaken for bad dandruff. The tell-tale signs are stubborn, greasy, yellowish scales, a visibly red scalp, and an itch that just won't quit.
This all happens because of an overgrowth of a yeast called Malassezia that lives on everyone's skin. For some people, the immune system decides to go to war with this yeast, triggering the inflammation that causes all the trouble. You’ll often see it pop up in oily areas beyond the scalp, like the sides of the nose, ears, or chest.
While Seborrheic Dermatitis doesn't directly kill hair follicles, the constant inflammation and the intense scratching that comes with it can definitely cause temporary hair shedding. You can learn more about Seborrheic Dermatitis in our detailed guide to get a handle on it. The bottom line? Calm the inflammation, and you can stop the associated hair fall.
Folliculitis: When Follicles Get Infected
Ever found small, sore, pimple-like bumps on your scalp? That’s likely Folliculitis, which is exactly what it sounds like: inflammation of the hair follicles themselves. It’s usually caused by a bacterial or fungal infection that sneaks in, often through tiny breaks in the skin from scratching, shaving, or even wearing a tight hat too often.
Here’s what to look for:
- Small red bumps or white-headed pimples scattered on the scalp.
- Tenderness, soreness, or itching right around the bumps.
- In worse cases, these can morph into larger, pus-filled boils.
Thankfully, most cases are superficial and go away with better hygiene or topical treatments. But if it becomes deep or keeps coming back, folliculitis can damage the follicle enough to cause small, permanent bald spots. It's a perfect example of how a "minor" infection can become a real problem for your hair density.
Alopecia Areata: An Autoimmune Mix-Up
Alopecia Areata is the classic case of non-scarring inflammatory hair loss. It’s an autoimmune condition where the body gets its signals crossed and your own immune system attacks healthy hair follicles. This assault slams the brakes on hair growth, leading to smooth, round, completely bald patches that can show up overnight.
The condition is notoriously unpredictable. It can be a single coin-sized patch or involve much more extensive loss. Sometimes the hair grows back on its own, only to fall out again later. What’s unique is that the scalp skin itself usually looks perfectly normal—no redness, no scales, just a sudden absence of hair.
Alopecia Areata is far more common than you might think. It's estimated to affect about 2% of people worldwide. The numbers are also climbing, with cases growing from roughly 21.7 million in 1990 to 32.4 million in 2019—a jump of nearly 49%.
Lichen Planopilaris: A Scarring Condition with a Burn
Now we're getting into the more serious territory of scarring alopecias. Lichen Planopilaris (LPP) is a condition you need to act on fast. It triggers a wave of inflammation that literally destroys the hair follicle, replacing it with scar tissue. Once that happens, the hair loss is permanent.
People with LPP often describe more than just itching—they feel a distinct burning sensation, pain, or sharp tenderness on their scalp. You might see redness and scaling clustered right around the base of individual hairs. As it progresses, it leaves behind shiny, smooth bald patches where the follicles used to be. Prompt medical treatment is essential to stop the inflammatory attack and save the hair you still have.
Frontal Fibrosing Alopecia: A Telltale Pattern of Loss
Consider Frontal Fibrosing Alopecia (FFA) a specific type of Lichen Planopilaris with a very distinct calling card. It almost always affects the frontal hairline, causing it to slowly and steadily recede in a band-like pattern. It’s also notorious for causing the loss of eyebrows.
FFA is seen most often in post-menopausal women, but men can get it, too. The affected skin often looks pale and unusually smooth. Just like with LPP, the entire goal of treatment is to halt the inflammation before it wipes out more follicles for good. If you notice your hairline creeping backward and your eyebrows thinning out, that's a major red flag to get a professional diagnosis.
Learning to Read Your Scalp's Warning Signs
Your scalp rarely suffers in silence. It sends out pretty clear signals when inflammation is brewing, but it's all too easy to brush them off as just a "bad scalp day." Learning to recognize these cues is the single most important first step you can take to stop inflammatory hair loss before it gets worse.
Think of yourself as a detective for your own health. By paying attention to what you see and feel, you're gathering critical evidence. This history is gold when you eventually talk to a doctor, helping them connect the dots much faster to reach the right diagnosis.
Let’s break down the clues your scalp might be sending you.
Visual Clues You Can See
The first thing to do is a simple visual check. Grab a mirror, stand under some good light, and part your hair in a few different spots. You're looking for any sign that the environment for your hair follicles has turned hostile.
Here’s what to look for:
- Persistent Redness: A healthy scalp should be a calm, pale color. If you're seeing widespread pinkness or angry-looking red patches that don't go away, that’s a classic sign of inflammation.
- Flakes or Scales: What kind of flakes are you seeing? Are they small and white like a light dusting of snow, or are they larger, greasy, and yellowish? The type of flaking can point toward very different culprits, from simple dryness to something more complex like seborrheic dermatitis.
- Pimple-like Bumps: Small, tender red bumps or even little whiteheads (pustules) popping up on your scalp often signal folliculitis. This is a direct sign that the hair follicles themselves are infected and inflamed.
These visual signs are your scalp's way of showing you that a battle is being waged right on the surface.
Physical Sensations You Can Feel
Inflammation isn't just something you see; it's something you feel. These physical symptoms are often the most frustrating because they directly impact your daily comfort and scream that the inflammatory process is active. Don't ignore them.
Pay close attention to any new or persistent feelings on your scalp. An itch that won’t quit, a burning feeling, or soreness when you touch your head are direct communications from your nervous system that something is wrong.
Common sensations to take note of include:
- Constant Itching (Pruritus): This isn't just a fleeting tickle. We’re talking about a distracting, persistent itch that makes you want to scratch constantly—which, unfortunately, just adds fuel to the inflammatory fire.
- Burning or Stinging: Some conditions, particularly the scarring alopecias like Lichen Planopilaris, are notorious for causing a distinct burning or stinging pain. It's a very specific and uncomfortable feeling.
- Tenderness or Soreness: Does your scalp hurt when you touch it, brush your hair, or even just rest your head on a pillow? That kind of sensitivity is a major red flag for deep-seated inflammation.
Changes in Your Hair
Ultimately, the chaos on your scalp is going to affect your hair. When you start connecting the dots between your scalp's condition and how your hair is behaving, you can be more certain that the two issues are linked.
If you've been wondering how to tell if your hair is thinning, observing these changes alongside your scalp symptoms is a huge piece of the puzzle. You can learn more by checking out our guide on how to tell if my hair is thinning.
Look for these hair-related signs:
- Increased Shedding: Are you finding way more hair on your brush, in the shower drain, or on your pillow? Inflammation can literally shock follicles into the shedding phase way too early.
- Hair Breakage: Inflamed follicles often produce weaker, more brittle hair shafts that just can't take the stress. They snap off easily, sometimes very close to the scalp.
- Noticeable Thinning: Over time, that one-two punch of increased shedding and weaker new growth leads to a visible drop in hair density, either all over your head or in specific patches.
To help you put these clues together, here is a quick reference table.
Decoding Your Scalp's Symptoms
This table summarizes some of the most common symptoms and the inflammatory conditions they're often linked to. Remember, this is just a guide—many conditions share symptoms, and only a professional can give you a definitive diagnosis.
| Symptom (What You See or Feel) | Possible Associated Condition(s) |
|---|---|
| Itching, Greasy Yellowish Flakes, Redness | Seborrheic Dermatitis |
| Pus-filled Bumps (Pustules), Red Bumps | Folliculitis |
| Smooth, Round Patches of Complete Hair Loss | Alopecia Areata |
| Intense Itching, Burning, Soreness, Redness Around Follicles | Lichen Planopilaris (scarring alopecia) |
| Red, Scaly, Coin-shaped Sores, Scarring | Discoid Lupus Erythematosus (scarring alopecia) |
| General Redness, Itching, and Diffuse Shedding | Can be a sign of many non-scarring inflammatory issues |
By systematically observing these visual, physical, and hair-related signs, you transform vague worries into concrete information. This empowers you to walk into a specialist's office with a clear and detailed account of your experience, ready to find a solution.
Your Action Plan for Combating Inflammatory Hair Loss

Alright, you understand the problem. Now, let’s talk about solutions. Tackling inflammation on scalp hair loss isn't about finding a single magic bullet; it's about building a smart, multi-pronged strategy. Think of it as a partnership between you and your doctor, combining powerful medical treatments with consistent at-home care to calm your scalp and give your hair a real chance to recover.
The goal is simple: put out the inflammatory fire. Once that's under control, you can focus on creating a healthy environment where your hair follicles can finally thrive.
Starting with Medical Interventions
When your scalp is actively inflamed and angry, the first order of business is getting a dermatologist involved. They can prescribe targeted medical treatments designed to get the situation under control quickly and effectively.
Often, the first line of defense is corticosteroids. These can come in various forms—topical creams, foams, or even injections directly into the most irritated spots on your scalp. For more severe, widespread cases, oral steroids might be necessary. They all work by suppressing the immune cells that are mistakenly attacking your hair follicles, essentially telling them to stand down.
For more specific autoimmune conditions like alopecia areata, doctors might turn to newer immunomodulators. These drugs are a bit more sophisticated, targeting the precise inflammatory signals causing the problem, which can offer a more focused way to restore peace to your scalp.
Building Supportive Habits at Home
While your doctor’s treatments are doing the heavy lifting, the habits you build at home lay the groundwork for long-term success. These daily practices can help reduce background inflammation and keep future flare-ups at bay.
It can start with something as simple as your shower routine. Using the right medicated shampoo can make a world of difference. For instance, products with ketoconazole are fantastic for controlling the yeast linked to seborrheic dermatitis, a very common trigger for an itchy, inflamed scalp. We break down exactly how they work in our guide to ketoconazole shampoo for hair loss.
Think of at-home care as tending to the "soil" of your scalp. By keeping it clean, balanced, and nourished, you're creating the perfect conditions for the "seeds"—your hair follicles—to grow once the immediate threat is gone.
Another huge piece of the puzzle is adopting an anti-inflammatory diet. It’s true: what you eat directly impacts your body's overall level of inflammation.
Try to load up your plate with foods rich in:
- Omega-3 Fatty Acids: Think salmon, walnuts, and flaxseeds. These are proven to help lower inflammatory markers in the body.
- Antioxidants: Berries, leafy greens, and other colorful veggies are packed with them, helping to fight the oxidative stress that fuels inflammation.
- Lean Proteins: These are the essential building blocks for strong, healthy hair.
At the same time, it's a good idea to cut back on things that can trigger inflammation for many people, like processed foods, excess sugar, and dairy.
Exploring Advanced and Regenerative Therapies
For those who want to go beyond just managing symptoms, regenerative therapies are an exciting frontier. These treatments don't just calm the scalp—they aim to actively stimulate and support the hair follicles themselves.
One of the most promising options is Platelet-Rich Plasma (PRP). This therapy uses the concentrated growth factors from your own blood to help heal damaged scalp tissue and coax dormant follicles back into the growth phase. Exploring options like Platelet-Rich Plasma (PRP) treatments can be a proactive way to regenerate follicles and improve the scalp environment, rather than just reacting to damage after the fact.
It’s also important to be realistic, especially when dealing with certain conditions. Scarring alopecias like lichen planopilaris can cause permanent follicle damage. With these conditions, the chronic inflammation can unfortunately destroy the follicle’s stem cells for good, making regrowth impossible. This is why early and aggressive treatment is absolutely critical—the main goal becomes stopping the progression and saving the hair you still have.
Knowing When to See a Doctor
While at-home care and over-the-counter products are fantastic for managing mild scalp issues, they have their limits. The single most important step you can take for your hair is knowing when to stop guessing and bring in a professional, especially when you're dealing with inflammation on scalp hair loss.
What might look like simple dandruff or a minor irritation could actually be a sign of something more complex brewing beneath the surface. If your own efforts just aren't cutting it, it's time to call in an expert.
Critical Red Flags to Watch For
If you notice any of the following, don't wait for things to get worse. It’s a clear signal to book an appointment with a dermatologist or a hair loss specialist.
Pay close attention to these warning signs:
- Rapid or Patchy Hair Loss: Are you suddenly shedding clumps of hair? Or have smooth, bald patches appeared out of nowhere? This needs immediate attention.
- A Painful Scalp: A scalp that feels tender, sore to the touch, or has a constant burning sensation points to significant inflammation—far more than a simple shampoo can handle.
- No Improvement: You’ve been consistent with medicated shampoos and lifestyle changes for weeks, but nothing’s changing, or worse, your symptoms are escalating.
Making that appointment can feel like a big step, but it’s honestly the most powerful move you can make. Early, accurate diagnosis is everything when it comes to saving your hair, particularly with scarring conditions where follicle damage can become permanent.
What to Expect at Your Consultation
Don't worry, the consultation process is usually pretty straightforward. The doctor will start with a thorough examination of your scalp, often using a special magnifying tool called a trichoscope to get a high-definition look at your follicles and skin.
In some situations, they might recommend a scalp biopsy to get a definitive answer. It’s a quick procedure where a tiny tissue sample is taken, giving the lab a window into what’s happening at a cellular level. It’s the best way to get a precise diagnosis and build a treatment plan that’s actually right for you.
Answering Your Top Questions
When you're dealing with scalp inflammation and hair loss, it's natural to have a lot of questions. Let's break down some of the most common ones with straightforward answers to help you figure out your next steps.
Can Stress Really Cause Scalp Inflammation and Hair Loss?
It absolutely can. When you're under intense stress, your body kicks into high gear, releasing hormones that ramp up inflammation everywhere—including your scalp. This can easily flare up conditions like seborrheic dermatitis or even trigger a sudden shedding event known as telogen effluvium.
That's why managing stress is more than just a lifestyle tip; it's a core part of any treatment plan for inflammation on scalp hair loss. Things like mindfulness, regular exercise, and getting enough sleep help create a calmer internal environment, which is exactly what your scalp needs to heal.
Will My Hair Grow Back After Inflammatory Hair Loss?
This is the big question, and the answer really hinges on the type of inflammation you're dealing with. For non-scarring conditions like alopecia areata or a temporary bout of folliculitis, the hair follicles are usually just dormant, not destroyed. Once you get the inflammation under control, there's a very good chance your hair can grow back fully.
Scarring alopecias, like lichen planopilaris, are a different story. Here, the inflammation is so aggressive that it permanently damages the hair follicle.
With scarring alopecias, the goal of treatment shifts. We focus on halting the inflammation to stop further hair loss and save the hair you still have. This makes getting an early, accurate diagnosis absolutely critical.
Are There Specific Foods That Can Help or Hurt Scalp Inflammation?
Your diet isn't a silver bullet, but it can be a powerful ally. Adopting an anti-inflammatory eating plan can help lower your body's overall inflammation levels, which definitely benefits your scalp health.
Think about adding more of these to your plate:
- Omega-3 Fatty Acids: Salmon and walnuts are packed with these, which are famous for their ability to cool down inflammatory responses.
- Antioxidants: Load up on berries and leafy green vegetables to fight the oxidative stress that fuels inflammation.
- Lean Proteins: These are the essential building blocks your body needs to grow strong, healthy hair.
On the flip side, you might find it helpful to cut back on processed foods, refined sugars, and for some people, dairy. These can be common triggers for inflammation, so it's worth paying attention to how your body and scalp feel when you eat them.
At PRP For HairLoss, we know that getting to the root cause of your hair loss is the only way to find a solution that works. To learn more about advanced treatments and how to take back control of your scalp health, visit us at https://prpforhairloss.com.

Leave a comment