Navigating hair loss can feel overwhelming, and the first question is always the same: what's causing it? When we look at alopecia areata vs androgenetic alopecia, we're dealing with two completely different culprits behind the hair fall.
Think of it this way: Alopecia Areata is an autoimmune condition where your body mistakenly attacks your hair follicles, causing sudden, patchy hair loss. On the other hand, Androgenetic Alopecia—what most people call male or female pattern baldness—is a slow, predictable thinning driven by your genes and hormones.
Understanding Your Hair Loss: The Key Differences
Hair loss isn't a one-size-fits-all problem. Alopecia areata and androgenetic alopecia are two of the most common diagnoses, but they couldn't be more different. Mistaking one for the other can send you down a path of frustrating and ineffective treatments.
Grasping their core distinctions is the first step toward regaining control. One is an unpredictable ambush from your own immune system, while the other is a slow, inherited process that unfolds over years.
Their impact and who they affect also tell different stories. Alopecia areata can strike anyone at any age and affects about 2% of the global population, which is roughly 160 million people. It often first appears in younger adults, typically between ages 30-49.
In sharp contrast, androgenetic alopecia is a genetic condition that becomes much more common with age. It affects a staggering 80% of Caucasian men by age 70. This is why getting the right diagnosis from the start is so critical.
To help you get a clearer picture of what you might be experiencing, here’s a straightforward breakdown of their defining features.
Key Differences At a Glance: Alopecia Areata vs Androgenetic Alopecia
This table is a quick cheat sheet for telling the two conditions apart based on what you’re seeing and experiencing.
| Feature | Alopecia Areata | Androgenetic Alopecia |
|---|---|---|
| Primary Cause | An autoimmune response; the body attacks its own hair follicles. | A genetic predisposition and sensitivity to the hormone DHT. |
| Pattern of Loss | Round or oval bald patches that can appear anywhere on the body. | Predictable patterns; a receding hairline and thinning crown in men. |
| Onset Speed | Sudden and often rapid, with patches appearing over days or weeks. | Gradual and slow, developing over many months or years. |
| Associated Signs | A smooth, non-scarred scalp in bald areas; sometimes nail pitting. | Hair miniaturization (thinner, weaker strands); no inflammation. |
Knowing these fundamental differences is everything, as each condition demands a unique game plan for management and treatment. While this gives you a solid starting point, you can learn more about what causes hair loss to get deeper clarity on your specific situation.
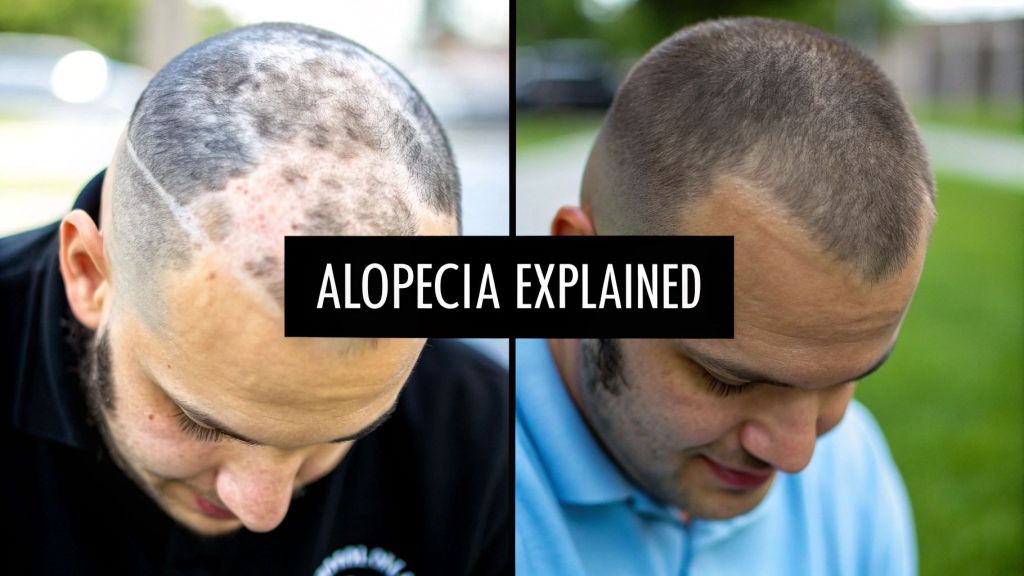
The Reality of Alopecia Areata: When Your Body Turns on Itself
At its core, alopecia areata (AA) is a case of mistaken identity. Your immune system, which is supposed to be your personal bodyguard, gets confused and starts attacking your own healthy hair follicles. It’s an autoimmune condition where the body’s defenses go on the offensive against the very structures responsible for growing hair.

This internal conflict causes inflammation that essentially puts the hair follicle into a dormant state. The result? Sudden, often rapid, hair loss. You’ll typically see smooth, round, or coin-sized bald patches pop up on the scalp, face, or anywhere else on the body. This is a world away from the slow, predictable thinning of male pattern baldness; AA is all about abrupt and erratic changes.
The Unpredictable Journey of Alopecia Areata
Living with alopecia areata is like living with constant uncertainty. Hair might fall out in one spot, start to grow back, and then disappear from a completely different area. This unpredictable cycle is one of the most difficult parts of the condition, making it impossible to know what the next month holds.
Alopecia areata isn't just one thing—it's a spectrum. The three main types show just how different it can look:
- Alopecia Areata (Patchy): The most common form, marked by one or more coin-sized bald spots.
- Alopecia Totalis: This is when all the hair on the scalp is lost completely.
- Alopecia Universalis: The most extensive form, resulting in the total loss of all body hair, including eyebrows and eyelashes.
The good news, if you can call it that, is that the hair follicles in alopecia areata aren't permanently destroyed. They're just dormant, put on pause by the immune system. This is why hair can, and often does, regrow on its own, sometimes even years later.
This condition is more widespread than people think. It's a major autoimmune disorder that affects roughly 2% of the global population—that's about 160 million people. While it can appear at any age, it most commonly starts between the ages of 30 and 49. Interestingly, recent data shows a rising trend, with new cases jumping by over 49% between 1990 and 2019. You can dive deeper into the numbers in this detailed research from PMC.
More Than Just Hair Loss
To really get what alopecia areata is about, you have to look past the physical symptoms. The emotional and psychological weight can be crushing. Losing your hair so suddenly can shake your identity, shatter your self-esteem, and make social situations feel daunting, often leading to anxiety and depression.
Managing the condition usually means trying to calm down the overactive immune response. For example, doctors often use topical or injected corticosteroids to reduce the inflammation right at the follicle. The goal is to suppress the local immune attack long enough for the hair to start growing again. Our guide on the relationship between corticosteroids and hair loss explains this common treatment strategy in more detail.
Ultimately, dealing with alopecia areata is a personal journey. It’s a condition that forces resilience in the face of the unknown and shines a light on how closely our appearance is tied to our sense of self. Understanding this human experience is just as important as knowing the biology when comparing alopecia areata vs androgenetic alopecia.
Androgenetic Alopecia: The Genetics of Pattern Hair Loss
While alopecia areata is an unpredictable autoimmune attack, androgenetic alopecia (AGA) follows a much clearer, inherited script. You probably know it as male or female pattern baldness. It's easily the most common type of hair loss on the planet, and its progression is slow, steady, and driven entirely by your genes and hormones.
Unlike the sudden patches that show up in alopecia areata, androgenetic alopecia is a gradual process of follicular miniaturization. Picture your hair follicles as tiny factories. If you have a genetic sensitivity, a hormone called dihydrotestosterone (DHT) starts to shrink these factories over time. They begin producing thinner, weaker, and shorter hairs until, eventually, they just shut down for good.
This isn’t some random occurrence; it’s a journey hardwired right into your DNA. The numbers really tell the story of its genetic roots. AGA affects an estimated 80 million people in the United States alone—that’s 50 million men and 30 million women. The chances of seeing it increase with age, affecting about 16% of men aged 18-29 and climbing to nearly 80% of Caucasian men by age 70. For a closer look, you can find more hair loss statistics on NCOA.org.
The Blueprint for Male Pattern Baldness
In men, androgenetic alopecia almost always follows a predictable map called the Norwood scale. This scale clearly outlines the typical stages of hair loss, giving us a reliable way to track how it’s advancing.
The whole process usually starts with subtle changes:
- A Receding Hairline: The first sign is often a slight recession at the temples, which creates that classic "M" shape.
- Thinning at the Crown: At the same time or soon after, you might notice thinning at the vertex, which is the crown of your head.
- Merging of Bald Areas: Over many years, the receding hairline and the thinning crown slowly expand until they meet, leaving that familiar patch of hair only on the sides and back of the head.
This progression is so consistent because the follicles on the top of the scalp are genetically programmed to be far more sensitive to DHT than the ones on the sides and back. This is a huge differentiator when comparing alopecia areata vs androgenetic alopecia, since AA can pop up absolutely anywhere.
How Androgenetic Alopecia Affects Women
For women, the story unfolds a bit differently. Female pattern hair loss is typically more spread out and is classified using the Ludwig scale. Instead of a receding hairline, women usually first notice a gradual widening of their part.
The thinning becomes most apparent across the top and crown of the scalp, but the frontal hairline often stays right where it is. Ponytails might feel less dense, and you might see more of your scalp under bright lights. This widespread thinning, rather than distinct bald spots, is the classic sign of AGA in women.
The key takeaway here is that androgenetic alopecia isn't an "attack" on your follicles. It's a slow, genetically predetermined shrinking process. Its predictable nature is what truly sets it apart from the chaotic and sudden loss you see in alopecia areata.
Getting to the root cause is everything for effective management. Because AGA is hormonal and genetic, treatments are designed to interfere with this specific process—either by blocking DHT or by stimulating those miniaturized follicles to get them back to work. For those wanting a deeper dive, you can learn more about what causes androgenetic alopecia in our detailed guide. Recognizing the slow, patterned nature of this condition is the first step toward choosing a treatment path that targets the real problem.
Comparing Symptoms and Diagnostic Clues
Telling the difference between alopecia areata and androgenetic alopecia often feels like playing detective. The clues are right there on your scalp, but you have to know what you're looking for. One condition can show up suddenly and erratically, while the other creeps in slowly over years, following a very predictable script.
The most fundamental difference is how they first appear. Alopecia areata typically bursts onto the scene as perfectly smooth, round, or oval bald patches that can seem to emerge overnight. On the flip side, androgenetic alopecia is a story of gradual thinning, not complete loss in distinct spots. This slow process, known as miniaturization, means hairs become finer and shorter long before the follicle gives up for good.
The Visual Cues: What to Look For
When you're examining your hair loss, the visual signs are your most immediate clues. Think of it as comparing a sudden, perfectly round clearing in a forest to the slow, overall thinning of the entire canopy. Each one tells a completely different story.
For alopecia areata, the key visual tip-offs are:
- Distinct Bald Patches: These are usually coin-sized, completely smooth, and can pop up on the scalp, beard, or even eyebrows.
- "Exclamation Point" Hairs: This is a classic sign. You'll see short, broken hairs that are narrower at the base than at the tip, often hanging around the edge of a new patch.
- Nail Changes: In some cases, people with AA might notice tiny dents or pitting on their fingernails—another subtle sign of an autoimmune response.
Androgenetic alopecia, however, paints a different picture entirely:
- Patterned Thinning: For men, this usually means a receding hairline (the classic "M" shape) and thinning at the crown. For women, it's more often a widening part and diffuse thinning across the top of the scalp.
- Miniaturized Hairs: Look closely, and you'll see weaker, finer, and shorter hairs mixed in with your normal strands. This is the tell-tale sign that follicles are shrinking.
A simple rule of thumb can be a huge help here: Sudden, patchy loss often points to Alopecia Areata; slow, patterned thinning suggests Androgenetic Alopecia. This single distinction is often the most powerful clue you have right from the start.
Progression and Timeline: A Race vs. a Marathon
The timeline of your hair loss is another critical piece of the puzzle. The progression of alopecia areata is notoriously unpredictable. It's a series of sprints and stops—patches can appear, regrow, and then show up somewhere else entirely without warning. For many, it's a frustrating cycle of loss and regrowth that can go on for years.
In stark contrast, androgenetic alopecia is a marathon. Its progression is slow, steady, and relentless if you don't intervene. It develops over months and years, often so gradually that many people don't even notice it until a significant amount of hair is already gone. This slow burn is a hallmark of its genetic and hormonal roots.
This decision tree gives you a simple way to visualize that first diagnostic question based on the speed of your hair loss.

As you can see, gradual thinning is the main road toward an androgenetic alopecia diagnosis, while more sudden loss means it's time to dig deeper for other causes.
To make these differences crystal clear, here’s a quick side-by-side checklist.
Symptom and Diagnostic Checklist
| Comparative Aspect | Alopecia Areata | Androgenetic Alopecia |
|---|---|---|
| Onset Speed | Sudden, often appearing over days or weeks. | Gradual, developing over many months or years. |
| Pattern of Loss | Round or oval patches of complete baldness. | Diffuse thinning, receding hairline, or crown loss. |
| Scalp Appearance | Smooth, non-scarred skin in bald spots. | Healthy scalp, but visible thinning between hairs. |
| Key Visual Sign | "Exclamation point" hairs at the edge of patches. | Hair miniaturization (finer, shorter, weaker hairs). |
| Associated Symptoms | Sometimes includes nail pitting or ridging. | Typically none, aside from the hair loss itself. |
| Common Diagnostic Tool | "Pull test" at the edge of a patch shows active loss. | Family history and following the Norwood/Ludwig scale. |
| Definitive Test | Scalp biopsy shows inflammation around the follicles. | Scalp biopsy shows shrunken (miniaturized) follicles. |
This table helps organize the clues, but a professional diagnosis is always the next step.
How a Professional Makes the Call
When you finally see a dermatologist, they'll combine all these visual clues with proven diagnostic methods to confirm what’s causing your hair loss. They’ll start with a thorough look at your scalp, often using a dermatoscope to get a magnified view of your hair follicles and the surrounding skin.
For suspected alopecia areata, a doctor might perform a "pull test." They gently tug on a small section of hair at the edge of a bald patch. If more than a few hairs come out easily, it’s a strong sign of active hair loss from AA.
With androgenetic alopecia, the diagnosis often leans heavily on your personal and family medical history. A clear pattern of hair loss that matches the Norwood scale (for men), paired with a family history of baldness, is usually enough to make a confident diagnosis. In trickier cases where the signs are muddled, a doctor might recommend a scalp biopsy for hair loss. This quick procedure provides a definitive answer by showing inflammation around the follicle (a sign of AA) or follicle miniaturization (a sign of AGA) under a microscope.
Choosing the Right Treatment Path
Figuring out the right hair loss treatment can feel overwhelming. It’s not a one-size-fits-all situation, especially when you’re dealing with two completely different conditions like alopecia areata and androgenetic alopecia. One requires calming down an internal battle, while the other is all about managing your genetic hand.

At its heart, treating alopecia areata is about getting your immune system to call a truce on your hair follicles. For androgenetic alopecia, the game plan is totally different—it's about fighting back against hormonal effects and waking up follicles that have gone dormant.
Taming the Immune System in Alopecia Areata
When tackling alopecia areata, the entire strategy is built around calming an overactive immune response right where it’s happening. You’re not trying to "cure" it, but rather manage the flare-ups and coax hair back during the quiet periods.
The most common game plans include:
- Corticosteroids: These are the heavy hitters for inflammation and usually the first thing a doctor will recommend. They come as topical creams, injections directly into the bald spots, or, for more widespread cases, oral pills to tamp down the immune system as a whole.
- JAK Inhibitors: As a newer class of drugs, Janus kinase (JAK) inhibitors are a big deal. They work by interrupting the specific signals the immune system uses to target follicles. Available as pills or topicals, they’ve shown real promise for people with extensive or particularly stubborn alopecia areata.
- Topical Immunotherapy: This is an interesting one. A specialist applies a chemical to the bald patches to cause a mild allergic reaction. The idea is to basically distract the immune system, getting it to focus on the new, minor irritation instead of your hair.
All these treatments are designed to manage the autoimmune process. Since the follicles themselves aren't permanently destroyed, there's always a chance for regrowth once the inflammation is under control.
Addressing Hormones in Androgenetic Alopecia
With androgenetic alopecia, we pivot from immune management to a two-pronged attack: hormonal intervention and follicle stimulation. The whole problem stems from a genetic sensitivity to DHT, so the best treatments either block that hormone or give the weakened follicles a serious boost.
The tried-and-true staples for AGA are:
- Minoxidil (Rogaine): This is a topical solution or foam that gets more blood flowing to the follicles. It essentially nudges miniaturized hairs back into their growth phase and helps them stay there longer, resulting in thicker, more substantial hair.
- Finasteride (Propecia): An oral pill for men, Finasteride gets right to the source by blocking the enzyme that turns testosterone into DHT. Lowering the DHT levels in your scalp stops the thinning process in its tracks and can even lead to significant regrowth.
Here’s the key takeaway: Alopecia areata treatments are about stopping an active assault. Androgenetic alopecia treatments are about defending your follicles from a slow, relentless hormonal siege.
As you weigh your options, you might also come across over-the-counter products like caffeine-based gel boosters designed to stimulate the scalp. While they aren't a frontline medical solution, they can complement a broader hair care strategy. To get a fuller picture of what’s out there, our guide on finding the best hair loss treatment can help you sort through your specific needs.
The Versatile Role of Platelet-Rich Plasma (PRP)
In the middle of all these specific therapies, Platelet-Rich Plasma (PRP) has made a name for itself as a compelling option that can help with both conditions, just in different ways. The procedure is straightforward: a small amount of your blood is drawn, spun in a centrifuge to concentrate the platelets, and then this "liquid gold" is injected back into your scalp.
PRP for Androgenetic Alopecia
For AGA, think of PRP as a powerful fertilizer for your scalp. The growth factors packed into the platelets get to work by:
- Reawakening Dormant Follicles: The injections can provide the jolt needed to revive shrunken, miniaturized follicles.
- Increasing Blood Supply: Better circulation means more oxygen and nutrients are delivered straight to the hair roots.
- Prolonging the Growth Phase: By nourishing the follicles, PRP helps hair grow thicker and for longer before shedding.
In this scenario, PRP directly counters the miniaturizing effect of DHT by strengthening the follicles from within.
PRP for Alopecia Areata
For AA, the mechanism is a bit more nuanced. The growth factors still give the follicles a boost, but they also bring powerful anti-inflammatory properties to the fight.
- Reducing Inflammation: PRP can help soothe the localized immune attack that’s causing the hair loss.
- Promoting Healing: The growth factors signal the body to repair tissue, creating a healthier, more stable environment for hair to grow back.
Here, PRP therapy is playing both offense and defense. It helps calm the autoimmune response while simultaneously giving follicles the resources they need to recover. This dual action is what makes it such an adaptable and promising treatment in the complex world of hair loss.
When to See a Doctor and What to Ask
https://www.youtube.com/embed/lWxjis_UDig
Deciding when to finally see a doctor about hair loss can feel like a big step. It’s easy to get caught in a “wait and see” cycle, but some signs are too important to ignore. Taking action is the only way to get a real diagnosis and start a treatment plan that actually works.
If you’re seeing sudden, dramatic hair loss—think clumps in the shower drain or bald patches that appear out of nowhere—it’s time to book an appointment. That kind of rapid change often points to an underlying condition like alopecia areata, which really benefits from early medical intervention. The same goes for any hair loss that comes with scalp issues like itching, burning, redness, or pain. That’s a clear signal that it’s more than just male pattern baldness.
On the flip side, if your hair loss is more of a slow, predictable thinning that looks a lot like your dad’s or grandpa’s, the situation isn't as urgent. This is the classic sign of androgenetic alopecia, and it gives you a bit more breathing room to weigh your options. You might even start with a proven over-the-counter product while you keep an eye on things.
Preparing for Your Appointment
Walking into your consultation prepared can completely change the outcome. Your dermatologist will have questions, but you need to have your own list ready, too. Think of it as a partnership for your hair health.
Before your appointment, get your story straight.
- Document Your Timeline: Make a note of when you first noticed the thinning or shedding and how it has changed over time. Is it gradual or did it happen in bursts?
- Review Your Family History: Think about the hair loss patterns on both sides of your family. This is a huge clue, especially for androgenetic alopecia.
- List Your Medications: Write down everything you take, including prescriptions, over-the-counter drugs, vitamins, and supplements.
The main goal of this visit is to get clarity. You should walk out of that office knowing exactly what’s causing your hair loss, why it’s happening, and what the next steps look like.
Key Questions to Ask Your Dermatologist
Once you're there, don’t hesitate to ask detailed questions. The more informed you are, the better the results you’ll get. Focus your questions on understanding your specific situation and the key differences between alopecia areata vs androgenetic alopecia.
Here are some essential questions to kick things off:
- Given my pattern of hair loss and history, what do you think is the most likely cause?
- Are there any specific tests, like a biopsy or blood work, that we need to do to be sure?
- Could you walk me through all of my treatment options, from creams and pills to procedures like PRP?
- What kind of results can I realistically expect from each of these treatments? How long will it take to see them?
- Is there anything I can do with my diet or lifestyle to help support the treatment?
Getting solid answers to these questions puts you in the driver's seat. It gives you the power to make an informed decision that truly fits your diagnosis, budget, and personal goals.
Common Questions Answered
When you're dealing with hair loss, questions are bound to come up. Let's clear up some of the most common points of confusion when comparing alopecia areata and androgenetic alopecia.
Can Stress Cause Either Condition?
This is a big one. While a major shock or period of intense stress can cause a separate issue called telogen effluvium (a temporary shedding of hair), its connection to our two main conditions is more nuanced.
For alopecia areata, think of extreme stress as a potential spark. It doesn't cause the condition, but in someone who is already genetically wired for it, a stressful event might trigger the autoimmune response that leads to hair loss.
Androgenetic alopecia, on the other hand, is driven by genetics and hormones, not stress. That said, chronic stress isn't exactly helping. It can potentially accelerate the thinning process if you're already on that path.
Is Hair Regrowth Permanent After Treatment?
The answer really hinges on which type of alopecia you have. For alopecia areata, treatments can absolutely bring hair back. But because it's an autoimmune condition, there's no guarantee it will stay. The disease can have unpredictable cycles, meaning new patches could appear later on.
With androgenetic alopecia, treatments like Minoxidil or Finasteride are more of a long-term management plan. They work for as long as you use them. Stop the treatment, and the genetic and hormonal drivers of hair loss will pick right back up where they left off.
Key takeaway: Treatments for alopecia areata are about calming an immune response that might flare up again. Treatments for androgenetic alopecia are about putting up a continuous defense against a permanent genetic trait.
Can You Have Both at the Same Time?
It’s not common, but yes, you absolutely can. A man could be experiencing the typical gradual thinning of male pattern baldness and then suddenly develop the distinct, round bald patches of alopecia areata.
This kind of dual diagnosis really needs an expert eye. A dermatologist would have to create a two-pronged treatment plan to tackle both issues at once—one strategy for the autoimmune attack and another for the hormonal thinning.
At PRP For HairLoss, we know that getting to the root cause of your hair loss is the critical first step. It's the only way to find a solution that's right for you. To learn more about your options, including advanced treatments like Platelet-Rich Plasma, come see us at https://prpforhairloss.com.
Leave a comment