It’s a frustrating moment, isn't it? Finding more hair in your brush or on your pillow than usual. While we often point the finger at stress, genetics, or diet, a surprising number of common prescriptions could be the real culprit behind your thinning hair. It's called drug-induced alopecia, and while it's a distressing side effect, understanding the connection is the first step toward getting things back on track. Hair loss is a complex issue, and it's worth remembering that besides medications, there are other essential causes of thinning hair in women that could be at play.
We're going to dive into the world of common medications that cause hair loss, looking at not just which drugs are the problem, but why they do it. More importantly, we'll talk about practical steps you can take to manage the situation without putting your health at risk. We’ll break down eight major categories, covering everything from chemotherapy drugs and blood thinners to antidepressants and beta-blockers. Our goal is to arm you with the specific, useful information you need to have a real conversation with your doctor and take back control of your hair's health.
1. Chemotherapy Drugs (Antineoplastic Agents)
When people think of medications that cause hair loss, chemotherapy drugs are usually the first to come to mind. Their powerful, systemic effects make them stand out. These drugs, known as antineoplastic agents, are designed to go after and destroy rapidly dividing cancer cells. The catch is that this mechanism can't tell the difference between a cancer cell and other fast-growing cells in your body, like the ones in your hair follicles.
This "friendly fire" leads to a specific type of hair loss called anagen effluvium. It happens during the anagen, or active growth phase, of the hair cycle, causing a sudden and often dramatic shed. How severe it gets really depends on the specific drug, the dosage, and how long the treatment plan lasts. For example, breast cancer patients on a common AC-T regimen (Adriamycin, Cyclophosphamide, and Taxol) often experience complete hair loss on their scalp, eyebrows, and eyelashes.
The Hair Loss & Regrowth Timeline
The journey of hair loss and regrowth during chemotherapy tends to follow a fairly predictable path. Knowing this timeline can help you manage your expectations and prepare for the changes.
This infographic breaks down the typical timeline for hair changes associated with chemotherapy treatment.
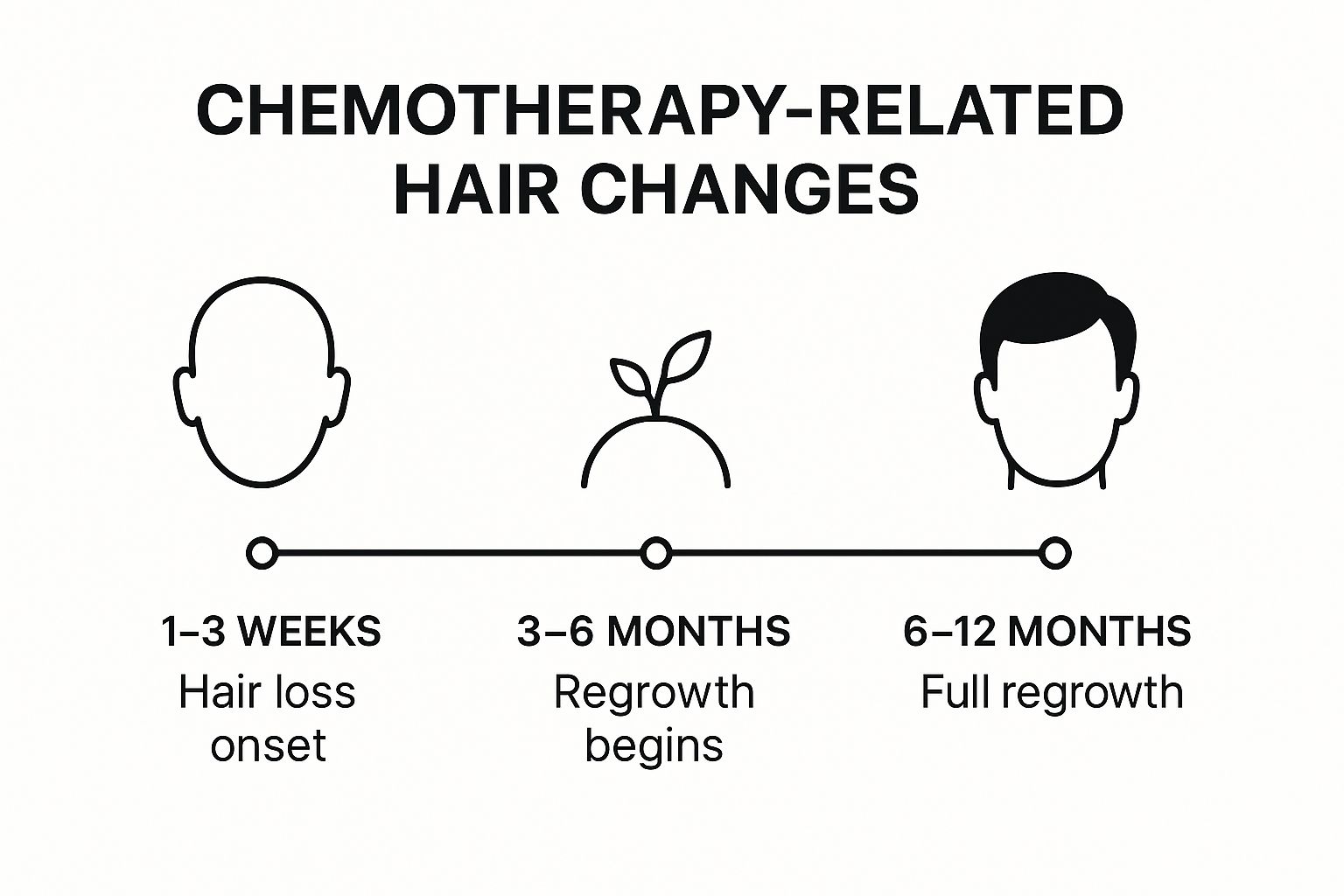
As you can see, while hair loss kicks in quickly after treatment starts, the regrowth process also begins relatively soon after it's over, with many people seeing a full recovery within a year.
Practical Steps to Manage Hair Loss
While it's often an unavoidable part of treatment, there are proactive steps you can take to manage chemotherapy-induced hair loss and protect your scalp.
- Consider Scalp Cooling: Cold caps or scalp cooling systems work by narrowing the blood vessels in your scalp. This reduces how much of the chemo drug reaches your hair follicles. Clinical trials have shown these devices can be 50-80% effective in preventing significant hair loss.
- Prepare in Advance: Getting a short haircut before treatment can soften the emotional blow of seeing large clumps of hair fall out. It’s also a good idea to shop for wigs, scarves, or hats beforehand so you have them ready when you need them.
- Gentle Scalp Care: As your hair thins, switch to a mild, sulfate-free shampoo. Once your hair is gone, be sure to protect your exposed scalp with sunscreen (SPF 30 or higher) to avoid sunburn.
For a better understanding of how these drugs work and what the experience is like for patients, the following video offers some valuable insights.
2. Anticoagulants (Blood Thinners)
Anticoagulants, which most of us know as blood thinners, are vital for preventing and treating blood clots in conditions like atrial fibrillation or deep vein thrombosis. But some of these medications, especially older ones like heparin and warfarin (Coumadin), are known as medications that cause hair loss by triggering a condition called telogen effluvium.

This kind of hair loss happens when a major stressor—like starting a potent new medication—pushes more hair follicles than usual into the telogen (resting) phase of the hair cycle. This premature rest leads to a diffuse, non-scarring shedding that you'd typically notice about two to four months after starting the treatment. The thinning is usually gradual and spread out across the entire scalp rather than in one spot. While newer direct oral anticoagulants (DOACs) like apixaban (Eliquis) and rivaroxaban (Xarelto) seem to cause this less often, they can still trigger hair loss for some people.
The Hair Loss & Management Timeline
The shedding from anticoagulants is often temporary and can be reversed, but managing it comes down to catching it early and talking to your doctor. For instance, a patient on long-term warfarin for stroke prevention might notice their hair gradually thinning over several months and could benefit from discussing other options.
Similarly, a post-surgical patient on short-term heparin might experience a temporary shed that clears up once the medication is stopped. The first step is just understanding the link between these drugs and the hair cycle. To dig deeper into this, you can learn more about other hair loss causes on prpforhairloss.com.
Practical Steps to Manage Hair Loss
If you think your blood thinner is causing hair loss, there are a few strategies that can help you manage the situation without risking your cardiovascular health.
- Consult Your Cardiologist: Never, ever stop taking your anticoagulant without your doctor's okay. Talk about your concerns with them; they might be able to switch you to an alternative medication that has a lower risk of this side effect.
- Document and Monitor: Keep a simple log and snap photos of your hair every few weeks. This will give you a clear timeline of the changes to share with your physician.
- Gentle Hair Care: Steer clear of harsh chemical treatments, tight hairstyles, and too much heat styling, which can put extra stress on your hair follicles. Use volumizing shampoos and conditioners to help your hair look fuller.
- Support Hair Health: Make sure your diet is rich in protein and iron, which are super important for hair growth. Ask your doctor if adding a biotin supplement (usually 2.5-5 mg daily) could help support your hair follicles.
3. Retinoids (Vitamin A Derivatives)
Retinoids, which are powerful derivatives of vitamin A, are incredibly effective for treating skin conditions like severe acne and psoriasis. Medications like isotretinoin (formerly Accutane) and acitretin work by regulating how skin cells turn over. But that same mechanism, especially in high doses, can mess with the normal hair growth cycle, making them potential medications that cause hair loss.

This disruption also leads to telogen effluvium, where way too many hair follicles get pushed into the telogen, or resting, phase. Instead of the usual 10-15% of follicles being at rest, a much larger percentage enters this phase, leading to noticeable, diffuse thinning a few months into treatment. The effect is usually dose-dependent; the higher the dose, the more likely you are to see shedding.
The Hair Loss & Reversal Process
Unlike the sudden loss you see with chemotherapy, retinoid-induced hair loss is generally more gradual and often reversible. For example, a teenager taking isotretinoin for cystic acne might notice more shedding between the second and fourth months of their treatment. Likewise, psoriasis patients on acitretin might experience thinning that can be managed by adjusting the dosage with their dermatologist's help. In cases where someone is taking too much vitamin A in supplements (over 10,000 IU daily), the hair loss typically stops within a few months of cutting back.
Practical Steps to Manage Hair Loss
While you should never change your prescribed medication dose without talking to your doctor, there are proactive steps you can take to support your hair's health during retinoid therapy.
- Avoid Excess Vitamin A: Don't take any extra vitamin A supplements or multivitamins with high levels of vitamin A while on prescription retinoids. This helps prevent a systemic overload.
- Gentle Hair Care Routine: Retinoids can make your skin and scalp dry. Use a gentle, moisturizing, sulfate-free shampoo and conditioner. Try to limit how often you use heat styling tools and avoid harsh chemical treatments like bleaching or perms.
- Support with Diet and Hydration: Make sure you're eating a balanced diet rich in hair-healthy nutrients like biotin (found in eggs, nuts, and seeds) and iron. Staying well-hydrated is also a big deal for your overall scalp and hair health.
4. Antidepressants (SSRIs and Tricyclics)
While they are essential for managing mental health, certain antidepressants are among the medications that can cause hair loss in a small fraction of users. This side effect is linked to drug classes like selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants, though scientists are still figuring out exactly why. The theory is that these drugs may prematurely push hair follicles from their active growth phase into a resting and shedding phase.
This process results in a condition called telogen effluvium. Unlike the rapid hair loss from chemo, this type is more of a gradual, diffuse thinning that you might notice two to four months after starting the medication or changing the dose. You rarely lose all your hair, but the increased shedding can definitely be distressing. For example, people taking fluoxetine (Prozac) or sertraline (Zoloft) have reported increased hair shedding that often resolves on its own or after they switch medications.
The Hair Loss & Management Timeline
The timeline for antidepressant-induced hair loss is a bit less predictable and really depends on the individual. The thinning often starts several months into treatment and can sometimes level off without you having to do anything. However, if the shedding is persistent or significant, tweaking the treatment plan can usually reverse the effect over the following months as your hair follicles get back to their normal growth cycle.
It's also really important to figure out if it's the medication causing the hair loss or an underlying condition. For instance, the stress and anxiety that led to treatment in the first place can trigger hair loss on their own. Understanding how these factors are related is key. You can learn more about the connection between anxiety and hair loss at prpforhairloss.com.
Practical Steps to Manage Hair Loss
If you suspect your antidepressant is causing your hair to thin, it's vital to talk to your healthcare provider about it without just stopping your medication cold turkey.
- Track Your Timeline: Keep a simple log of when you started your medication and when you first noticed more shedding. This information is gold for your doctor when trying to establish a link.
- Discuss Alternatives: Chat with your prescriber about your concerns. They might suggest switching to an alternative with a lower reported incidence of hair loss, like bupropion or mirtazapine, or just adjusting your current dose.
- Support Overall Health: Focus on eating a nutrient-rich diet and practicing stress-management techniques like meditation or exercise. This helps make sure your body has what it needs for healthy hair growth and minimizes other potential triggers for telogen effluvium.
5. Beta-Blockers (Antihypertensive Medications)
Beta-blockers are a go-to treatment for conditions like high blood pressure, angina, and anxiety. They work by blocking the effects of adrenaline, which slows the heart rate and brings down blood pressure. While they're great for your cardiovascular health, these medications can unfortunately contribute to hair loss in a small number of patients, typically affecting around 1-5% of people who take them.
This type of hair loss is another case of telogen effluvium, a diffuse thinning that happens when a lot of hair follicles get pushed into the telogen, or resting phase, way too early. It might be linked to the medication's impact on blood flow to the scalp or its subtle interference with the hormonal pathways that control the hair growth cycle. Older, non-selective beta-blockers like propranolol and metoprolol are more often linked to this side effect than the newer, cardioselective ones.
The Hair Loss & Management Timeline
Unlike the rapid hair loss seen with chemotherapy, beta-blocker-induced thinning is a slow burn. It usually starts 2-4 months after you begin the medication and shows up as increased shedding and less overall hair density, not complete bald patches. For example, someone taking propranolol for high blood pressure might notice more hair on their pillow or in the shower drain over several weeks, which can be upsetting.
The good news is that this condition is often reversible. If the beta-blocker is identified as the problem, a doctor might switch the patient to a different class of blood pressure medication, like an ACE inhibitor. Hair growth usually starts up again within a few months after stopping the offending drug, though it can take up to a year for your hair's density to fully return to what it was.
Practical Steps to Manage Hair Loss
If you think your beta-blocker is causing your hair to thin, it's really important to consult your doctor before making any changes. Here are some proactive steps to discuss and try.
- Discuss Alternatives with Your Doctor: Ask your cardiologist if switching to a more cardioselective beta-blocker (like atenolol or bisoprolol) is an option, as they might have a lower risk of causing hair loss. In some cases, a different class of medication, like an ACE inhibitor or an ARB, might be a good substitute.
- Support Follicle Health: Make sure your diet is packed with hair-supporting nutrients like iron, zinc, and protein. Using a scalp-stimulating shampoo with ingredients like caffeine can also help improve microcirculation to the hair follicles.
- Monitor Other Health Factors: Both thyroid conditions and beta-blocker use can affect your hair. Getting regular blood tests to check your thyroid function can help rule out or address other things that might be contributing to your hair loss.
6. Hormonal Medications (Contraceptives and Hormone Replacement)
Hormonal medications, like birth control and hormone replacement therapies, can have a big impact on the hair growth cycle. These drugs play with the body's hormonal balance, which can accidentally trigger or worsen hair loss in people who are already genetically predisposed to it. The main mechanism involves androgens, or male hormones, which can shrink hair follicles and lead to androgenetic alopecia.
The effect often comes down to the specific formula. For instance, birth control pills with a high androgen index can act like testosterone, leading to thinning hair. On the flip side, stopping hormonal contraceptives can cause a temporary shedding condition known as telogen effluvium, as your body readjusts. Similarly, testosterone therapy, used by both cisgender and transgender men, can speed up male-pattern baldness in those who are susceptible.
The Hormonal Link to Hair Changes
Understanding how hormones affect your hair is the key to managing this side effect. Any fluctuations, whether from starting, stopping, or changing medications, can throw the natural hair cycle out of whack. This is especially true for women who are planning a pregnancy and stop taking birth control, only to notice increased shedding—a condition often called post-pill telogen effluvium. The severity and type of hair loss are tied directly to the specific hormone, its dosage, and your individual sensitivity.
Recognizing this connection is the first step toward finding a solution that works for both your health needs and your hair.
Practical Steps to Manage Hair Loss
If you think hormonal medications are causing your hair loss, there are several proactive strategies you can discuss with your healthcare provider.
- Choose Low-Androgen Options: Look for birth control pills that contain progestins with low androgenic activity, such as desogestrel, norgestimate, or drospirenone (found in Yasmin or Yaz). These are less likely to cause hair thinning.
- Monitor Your Body's Response: Keep in mind that temporary shedding is pretty common when starting or stopping any hormonal treatment. If the hair loss keeps up for more than six months, you might consider adding topical minoxidil to help stimulate regrowth.
- Explore Non-Hormonal Alternatives: If hair loss is severe or a major concern for you, talk to your doctor about non-hormonal contraceptive methods like the copper IUD.
- Check Key Nutrient Levels: Hormonal changes can mess with your iron and ferritin levels, which are critical for healthy hair growth. Ask for a blood test to make sure your levels are in the optimal range.
7. Immunosuppressants and Biologics
Medications designed to suppress the immune system are lifesavers for treating autoimmune conditions like rheumatoid arthritis and preventing organ transplant rejection. However, by changing these complex immune pathways, these drugs can sometimes interfere with the hair growth cycle. Immunosuppressants like methotrexate and biologics like TNF-inhibitors are among the medications that cause hair loss by disrupting hair follicle cell division or creating an inflammatory environment.
This type of hair loss is usually telogen effluvium, a diffuse shedding caused by follicles entering the resting phase too early. The incidence varies a lot; for example, methotrexate is linked to a 1-3% rate of hair loss, while certain biologics can paradoxically trigger alopecia areata, an autoimmune form of hair loss. For some patients, like transplant recipients on cyclosporine, the effect can be mixed, causing their scalp hair to thin while increasing their body hair.
The Connection Between Immune Function and Hair
The relationship between your immune system and your hair follicles is a delicate one. When these medications dampen your immune response to treat a primary condition, they can sometimes disrupt the signals that keep your hair in its active growth phase. Understanding this connection helps explain why managing these side effects is so important.
For instance, a patient with Crohn's disease might notice their hair growth improves after switching from a broad immunosuppressant like azathioprine to a more targeted biologic. This highlights the different ways these drugs can affect hair follicles. It's also useful to know the difference between these drugs and other immune-modulating treatments. You can learn more about corticosteroids and hair loss on prpforhairloss.com to get the full picture.
Practical Steps to Manage Hair Loss
If you're taking an immunosuppressant and experiencing hair thinning, there are several effective strategies you can discuss with your doctor to help mitigate the issue.
- Supplement with Folic Acid: For those on methotrexate, studies have shown that taking folic acid (1-5 mg daily) can cut the risk of hair loss by 60-80% by counteracting the drug's effect on cell division.
- Discuss Dose Adjustments: If the hair loss is significant, ask your rheumatologist or specialist if lowering the dose or trying an alternative medication is a safe option for managing your underlying condition.
- Monitor Your Scalp: Keep an eye out for signs of alopecia areata, like distinct circular bald patches. Catching it early allows your doctor to adjust your treatment plan quickly.
- Support Follicle Health: Maintain a nutrient-rich diet with enough protein, iron, and zinc. You can also consider using topical minoxidil to stimulate your follicles and support regrowth during your treatment.
8. Anticonvulsants (Anti-Seizure Medications)
Anticonvulsants, mainly used to manage seizure disorders like epilepsy, are another class of medications that can cause hair loss. These drugs work by stabilizing electrical activity in the brain, but their systemic effects can interfere with the hair growth cycle. The link is particularly strong with certain older anti-seizure medications.
The hair loss you see with these drugs is typically telogen effluvium, where hair follicles are pushed into the resting phase too early, leading to diffuse shedding. This is often tied to the medication's impact on how your body metabolizes nutrients, specifically depleting levels of biotin, zinc, and folate—all of which are vital for healthy hair. Valproic acid (Depakote) is the most common offender, affecting up to 25% of users, but others like carbamazepine and phenytoin can also trigger hair thinning.
The Hair Loss & Regrowth Timeline
Hair changes from anticonvulsants often sneak up on you over several months of treatment. For example, a patient taking valproic acid for migraine prevention might not notice any thinning until three to six months into their therapy. The good news is that this hair loss is frequently dose-dependent and reversible.
If the medication is adjusted or switched, regrowth usually begins within a few months as the body's nutrient levels stabilize and follicles re-enter the anagen (growth) phase. Many patients who switch to newer alternatives like lamotrigine or levetiracetam report that their hair grows back significantly.
Practical Steps to Manage Hair Loss
While you should never stop an anticonvulsant without medical supervision, there are proactive strategies you can talk about with your doctor to lessen the hair loss.
- Nutritional Supplementation: Talk to your doctor about supplementing with key nutrients. Studies show that adding zinc (25-50mg), selenium (200mcg), and biotin (5mg) can be especially helpful for those on valproic acid. A daily multivitamin with a B-complex can also help counter general nutrient depletion.
- Dose Optimization: Ask your physician about therapeutic drug monitoring. This involves blood tests to make sure you're on the lowest effective dose of your medication, which can reduce the severity of side effects like hair loss.
- Consider Alternatives: If the hair loss is significant and causing you distress, discuss switching to another anticonvulsant. Drugs like lamotrigine and levetiracetam have a much lower chance of causing hair loss and can be great alternatives for many conditions.
If you're dealing with this side effect, it's important to look into all the available options. For those looking for comprehensive strategies, you can learn more about ways to stimulate hair growth on prpforhairloss.com.
Medications Causing Hair Loss: Comparative Overview
| Medication Type | Implementation Complexity 🔄 | Resource Requirements ⚡ | Expected Outcomes 📊 | Ideal Use Cases 💡 | Key Advantages ⭐ |
|---|---|---|---|---|---|
| Chemotherapy Drugs (Antineoplastic Agents) | High: Complex treatment protocols, dosage management | High: Requires medical supervision, scalp cooling devices | Significant, rapid hair loss; typically reversible post-treatment | Cancer patients undergoing chemotherapy | Potent cancer treatment; hair regrowth usually occurs post-therapy |
| Anticoagulants (Blood Thinners) | Moderate: Routine monitoring, dose adjustments | Moderate: Blood tests and physician consultation | Gradual, diffuse hair thinning; usually reversible | Patients on warfarin, heparin, or DOACs | Effective thrombosis prevention; hair loss often mild and temporary |
| Retinoids (Vitamin A Derivatives) | Moderate: Dose-dependent management | Moderate: Prescriptions, monitoring vitamin A intake | Mild to significant thinning; reversible after discontinuation | Acne and psoriasis patients on retinoids | Effective skin condition treatment; manageable hair loss with dose control |
| Antidepressants (SSRIs and Tricyclics) | Moderate: Medication trials and switches | Low to Moderate: Psychiatric monitoring | Mild diffuse thinning; often stabilizes or resolves | Patients needing ongoing depression treatment | Mental health prioritized; hair loss often mild and manageable |
| Beta-Blockers (Antihypertensives) | Low to Moderate: Medication choice and monitoring | Low to Moderate: Cardiological supervision | Mild diffuse thinning; usually reversible upon med change | Hypertension, heart conditions needing beta-blockers | Cardiovascular benefits; newer agents reduce hair loss risk |
| Hormonal Medications (Contraceptives & HRT) | Moderate: Hormone level and side effect monitoring | Moderate: Prescription and follow-ups | Temporary or accelerated pattern hair loss; varies individually | Women using contraceptives or hormone replacement therapy | Multiple formulations available; some improve hair growth |
| Immunosuppressants and Biologics | High: Disease management with dose adjustments | High: Specialist oversight and supplementation | Variable hair loss; often reversible or manageable | Autoimmune and transplant patients | Effective immune modulation; folic acid reduces certain side effects |
| Anticonvulsants (Anti-Seizure Medications) | Moderate to High: Dose and drug selection complexity | Moderate: Therapeutic drug monitoring and supplements | Mild to significant thinning, texture changes; often reversible | Epilepsy, bipolar disorder, migraine prevention | Seizure control prioritized; supplementation reduces hair loss risk |
Taking Control: Your Next Steps for Healthier Hair
Trying to figure out prescription drugs and their side effects can feel overwhelming, especially when those effects impact something as personal as your hair. In this guide, we've walked through a wide range of common medications that cause hair loss, from life-saving chemo agents and heart-protecting beta-blockers to everyday antidepressants and anticonvulsants. The big takeaway here isn't to panic, but to be informed. Understanding the "how" and "why" behind drug-induced alopecia is the first real step toward taking back control of the situation.
The main theme we've seen again and again is the disruption of the hair growth cycle. Often, a medication pushes follicles from the anagen (growth) phase into the telogen (resting) phase too early, which leads to telogen effluvium. For other drugs, like chemo, the impact is more direct, causing a sudden loss known as anagen effluvium. Recognizing these patterns empowers you to have a much more productive chat with your doctor.
Your Action Plan: A Proactive Approach
Knowledge is great, but it's what you do with it that counts. The real value is using what you've learned to stand up for your own health and well-being. Here are the most important, actionable steps you can take if you think your medication is making your hair thin.
-
Consult Your Doctor (First and Always): I can't say this enough. Never stop or change the dose of a prescribed medication without explicit medical guidance. Your prescription is there for a reason—to manage an underlying health condition. Make an appointment to discuss your concerns and use this article as a jumping-off point to ask specific questions about your treatment.
-
Discuss Alternatives and Adjustments: Ask your physician if a lower dose could help with the hair loss without making the medication less effective. Inquire about other drugs in the same class, or even different classes, that might not have the same side-effect profile. This kind of proactive conversation is your most powerful tool.
-
Focus on Foundational Health: While the medication might be the main trigger, your body's overall health plays a huge role in your hair's resilience. Make sure you're eating a balanced diet rich in iron, zinc, biotin, and protein. Managing stress through exercise or mindfulness can also help ease telogen effluvium, which is often made worse by stress. For those looking to support regrowth, exploring options like the right top supplements for hair loss can be a great next step.
Remember: For many of the medications we've talked about, the hair loss is temporary and reversible. Once the drug is stopped or changed, your follicles can and often do recover, getting back to their normal growth cycle.
Ultimately, managing your health is a balancing act. The information here is meant to give you the clarity you need to partner effectively with your doctor. By understanding which medications that cause hair loss might be relevant to you and what your options are, you shift from being a passive patient to an active participant in your healthcare journey. That proactive mindset is key to finding a solution that protects both your health and your hair.
If your hair loss persists or you're seeking a powerful, non-surgical solution to stimulate regrowth, it's time to explore what modern science can offer. At PRP For HairLoss, we specialize in Platelet-Rich Plasma therapy, a cutting-edge treatment that uses your body's own growth factors to rejuvenate dormant hair follicles and promote new, healthy growth. Discover how PRP For HairLoss can help you reclaim your confidence and restore your hair, even when medication is a necessary part of your life.

Leave a comment